All health and freedom are different: external and internal.
1.
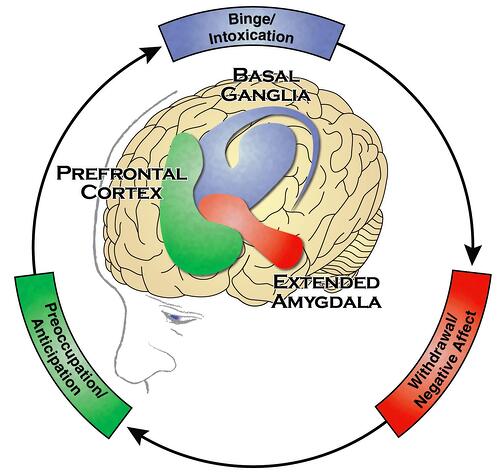
If some problem genes lurk in our genome, we are very likely to become addicts, moreover, relatively early, and our addiction will be difficult and hopeless. And if the genes are in order? This also does not guarantee anything: exposure to sufficiently high doses of substances endowed with addictive potential for a long time can make us addicted even with a "safe" genome. It doesn't matter with which set of cards we enter the addictive game. It doesn't matter what substance we pulled out of the temptingly shiny pile. In either case, we trigger neuroadaptive processes in certain brain structures. These processes, in a bad scenario, can form the so-called addictive cycle - the neurobiological essence of addiction.
2.
The human brain is made up of 86 billion neurons , "communicating" with each other with electrical signals through trillions of connections. These connections are called synapses. The synapse is composed of presynaptic and postsynaptic membranes. The space between the membranes is called the synaptic cleft. The presynaptic membrane, when a neuron is excited, secretes special substances - neurotransmitters. Glutamate, GABA, dopamine, serotonin, norepinephrine are neurotransmitters. The postsynaptic membrane has receptors for these substances. When a neurotransmitter molecule interacts with a receptor, a nerve signal is transmitted from one neuron to another. The main neurotransmitter of the reward system is dopamine.
All addictive substances are capable of producing feelings of pleasure. Yes, each of them also has its own specific effects. And, yes, the relationship between the intensity of pleasure and the magnitude of addictive potential is nonlinear (in other words, the substance that produces the most intense pleasure does not have to be ranked first in the addictiveness competition). But what makes a substance addictive is its ability to directly or indirectly affect the neurons of the reward system - the fundamental regulator of our behavior.
Our entire behavioral life fits into the formula trigger - behavior - reward . The nucleus accumbens is the key link in the reward system. Dorsal region of the striatum (lat. corpus striatum, pars dorsalis; English dorsal striatum ) - a key link in the formation of habits.
We experience reward both in the form of anticipation (wanting) and in the form of pleasure (liking). Wanting is a form of motivation generated by extensive neural systems, of which the mesolimbic dopamine system is a part. Liking is driven by the activity of smaller, more fragile neural systems, and seems to be dependent on enkephalins rather than dopamine. That wanting and liking are based on different mechanisms, first suggested by Kent Berridge and Terry Robinson. This hypothesis has been confirmed in both laboratory animals and humans. In the nucleus accumbens, approximately 90% wanting and 10% liking cells. Stop here and make sure that you understand the importance of the above: I want and like - these are different phenomena, and they are different even at the level of neurons. Now look at what exactly is important: the consumption of surfactants leads to the stimulation of only wanting neurons. Because of this, wanting intensifies, while liking not only does not intensify, but even gradually fades away.Thus, it can be said that addiction is not a problem of pleasure, but a problem of desire. Limbic power, there it is! - you will say in your hearts. And you will be right. Over the years, the hunger for psychoactive substances is getting stronger and stronger, and the pleasure from the use is less and less - here it is, the pulp of addictive neurodrama.

The theory of Berridge and Robinson in general boils down to this: addictive behavior arises from a functional mismatch between wanting and liking neurons: as surfactants are used, experimental mice (and people) want more and less like. And addicts see the only way to relieve wanting and increase liking in the continued use of surfactants, and they have to increase the dose to obtain the desired level of liking.
Dopamine systems are not just stimulated, but sensitized... Sensitization is expressed in changes in the morphology of neurons, for example, the shape and number of dendritic spines (recall the transcription factors NFκB and MEF2 from the previous chapter ). At the same time, wanting neurons become hyperreactive to surfactants and any signals promising drug cues: a Rhine wine glass, the smell of tobacco smoke, goa-trance music. In the future, with abstinence from PAS, sensitized neurons are not hyperactive all the time, of course. But they can become so in trigger situations. Once triggered, sensitization is very long lasting and possibly lifelong.
George Cub, Director of NIAAA, and Nora Volkow, Director of NIDA, developed and complemented Berridge and Robinson's concept. In studies led by them, it was shown that over-activation of neurons in the nucleus accumbens leads to neuroadaptive changes both within the reward system and in other brain systems (such as the amygdala and prefrontal cortex). Intra-systemic neuroadaptation concerns receptors: multiple excess dopamine releases caused by psychoactive substances lead to a compensatory decrease in the density of dopamine receptors on the postsynaptic membrane. Well, to somehow mitigate the dopamine attack. And what's wrong with that? And the fact that in the absence of surfactants, dopamine now binds to fewer receptors. At the level of subjective experiences, this leads to dissatisfaction, discontent, anhedonia.
Now about the dorsal striatum - the main structure of the habit circuitry. At some point, the need for the coveted substance becomes not just strong, but obsessive, compulsive: the person inside himself may be against the use, but as if no one is listening to him - there is a habit, strong and obsessive, and it needs to be maintained day after day. I do n’t want to , but it’s necessary , and it’s necessary as if it were living its own life. And the obsessive is necessarycontinues even after the transition to sobriety. For many months in a row, abstainers notice in themselves a vague, sometimes increasing need to do something and “fixate” on this or that behavior: they play video games for hours, get drunkenly immersed in TV shows, plunge headlong into sports, not quite realizing that they are following a compulsive call , about the same, which controlled their behavior during the use of surfactants.
So, the basis of a strong, irresistible attraction to surfactants is sensitization (morphofunctional changes) of dopamine neurons in the nucleus accumbens. At the same time, the level of pleasure (liking) not only does not grow, but even decreases. Parallel to this, the neurons of the dorsal striatum are involved, firmly integrating the search and use of surfactants into the habitual plan of life.
3.
In addition to the nucleus accumbens and the striatum, at some point the amygdala (lat.corpus amygdaloideum, eng.amygdala) appears on the addictive scene . This is a paired almond-shaped structure - one piece in each temporal lobe. The amygdala plays a key role in the formation of emotions (in particular, fear), remembering emotionally charged events and making decisions. As you can see, the amygdala is one of the top managers of our behavior.
Amygdala neurons contain a large number of receptors for corticotropin-releasing factor (CRF), norepinephrine, dynorphins - neurotransmitters of brain stress systems. CRF is a polypeptide that regulates hormonal, sympathetic and behavioral responses to stressors. Repeated administration of ethanol, cocaine, heroin, nicotine and other surfactants leads to changes in the neurotransmission of CRF in the amygdala in such a way that when these substances are canceled, CRF increases. Subjectively, the rise of the CRF is experienced as anxiety or aversion (the state of "don't like", "don't want").
Norepinephrine provides a behavioral response during stress by energizing neurons and focusing attention on stressors. CRF and norepinephrine activate each other.
Dynorphins are peptides tropic to κ-opioid receptors. Dynorphins mediate negative emotional states, including aversion, dysphoria, and depression. Dynorphins also increase the reward threshold and inhibit dopamine release. As well as CRF, the activity of dynorphins increases with the withdrawal of surfactants in persons with addiction.
Basically, here we can stop and think about this. Why do people drink most often? "I want to drink a hundred grams for appetite." Okay. Yet? "Well, the whole company is drinking, and that's why ..." Okay, more? “I’m tired, I’ve been under stress all day, the boss pissed off, my wife enrages, my back hurts ...” - is there such? The irony is this: while surfactants can actually release stress in the short term, they also activate the neurotransmission of CRF, norepinephrine, and dynorphins. This leads to the fact that the emotional state of addicts is deteriorating on the rise - for someone quickly and clearly, for someone slowly and barely noticeable. Alcohol, heroin, nicotine and other surfactants do not relieve stress, but intensify it, as they increase the level of CRF, norepinephrine and dynorphins.
This is best shown in a 5-minute cartoon.Nuggets: a kiwi bird walks on a flat surface, sees a drop, moves on. He sees another drop, tastes it. And suddenly everything around becomes sunny yellow, enchanting music appears, the kiwi takes off and flutters for a while with a blissful look. Then the drop effect wears off, the bird lands and moves on. From time to time she meets the same drops. Kiwi drinks them. Yellow color, music, flight. But each time the flight is shorter, the falls are more severe, and the environment - this is important - becomes more and more dark and gloomy. This is what the world looks like for a person with overly active stress systems of the amygdala: the world is gray and alien for him, a lot brings sadness, frightens or annoys. The unfortunate bird has only one thing to do: to find one more drop in order to return the ephemeral yellow light at least for a short time, without understanding,that the world is so blackened precisely because of these drops and that after each drop it will become even blacker.
Obviously, if you continue to use surfactants, changes in the stress systems of the amygdala will only intensify over the years. And if you stop? If you remove all surfactants, go through the withdrawal syndrome - will it be okay next? Fortunately, yes. But not at once. There is such a term: protracted abstinence. In Russian: subacute withdrawal symptoms. People who have been addicted to alcohol for 10, 15, 20 years, and then stop drinking, do not return so quickly to a comfortable emotional state - a sensitized amygdala takes months, and sometimes even years, to recover.
(It should be added that hyperactivation of the amygdala is also possible in other conditions, such as post-traumatic stress or chronic pain. These people have a higher addictive vulnerability and take longer to recover.)
4.
What could be worse than a negative emotional state due to a disheveled, frayed amygdala? The most unpleasant thing that I myself learned from my 15-year addictive experience is to be unreasonable in my own eyes. I couldn’t come to terms with the fact that I was smoking, but I also couldn’t quit. The discomfort we experience when our behavior doesn't align with our beliefs is what Leon Festinger called cognitive dissonance. True, the dissonance disappeared at the moment when, waking up in the morning, I did the coveted first puff. Everyone knows about Schrödinger's cat. Festinger's cat scratched, then not scratched my soul.
Under the influence of surfactants, dopamine transmission is suppressed not only in the reward system, but also in the prefrontal cortex. Because of this, executive functions deteriorate.: self-regulation, decision-making, flexibility in choosing and initiating actions, assignment of significance and error control. Further, neuroplastic changes also affect glutamatergic transmission. Impaired transmission of dopamine and glutamate to the prefrontal regions of the brain impairs their ability to resist strong urges or to stop using promptly. These effects explain why people with addiction may be sincere in their intention to stop using psychoactive substances and at the same time be unable to follow their decision.
five.
Everything that happens to the neurons of the basal ganglia, amygdala, prefrontal cortex due to the use of surfactants, is reflected in the desires, emotions, thoughts of a person, in the decisions he makes, in behavior and life. What exactly happens to neurons? We now know that: the expression of various transcription factors is enhanced, genes are activated, proteins are synthesized, the nerve cell undergoes morphological and functional changes, sensitizing to certain signals. These changes are called neuroplastic changes.
Neuroplasticity is the essence of learning. Our brain is not a static organ, but a complex, constantly changing system that can adapt to solving emerging problems. So, this is understandable, but what exactly gets sick in the brain during addiction? Is addiction a disease?
But there is no scientific consensus on the answer to this question yet. Yes, we can find the diagnosis of addiction syndrome among mental and behavioral disorders in the 10th revision of the International Classification of Diseases. We can find clinical guidelines for addiction treatment. And to conclude: since this diagnosis got into the ICD-10 and since it is treated with drugs, then this is a disease. On some formal grounds, addiction can be considered a disorder, I agree with that. Neuroscientist Mark Lewis disagrees. He put his disagreement in the subtitle of the book "The Biology of Desire", it sounds like this: "Addiction is not a disease." The debate about the nature of addiction captured me strongly, and I seem to be writing a separate book about it. Here I will only briefly note the following. Mark Lewis argues that everything that underlies addiction fits into the notion of learning:the brain neuroplastically adjusts to the tasks of searching for and using surfactants. We may have different attitudes to this learning, but this is precisely learning. Simply put,addiction is not something that the brain has become ill with, but something that it has learned . Even such serious supporters of the "brain disease theory" as George Cube and Nora Volkow in their research usually do not write "neuronal damage" - they write "neuroadaptive changes." These changes are extreme, Kent Berridge argues , and we have reason to view addiction as a disorder. But the same Kent Berridge and his colleague Terry Robinson in their publications on the neurobiology of addiction never talk about the pathology of neurons - they talk about the sensitization of neurons. In addition to the extreme positions in this scientific discussion, there are more balanced concepts, skillfully combining the features of both positions. So, Anke Snook suggestsconsider addiction as a normal phenomenon, within which there is sometimes a "disease-like stage".
Here I want to end with the words of Kent Berridge: “Maybe it’s fun to argue about the words, which ones best describe addiction. But, I think, arguments about words, for example, about whether to say "brain disease", and not about the real characteristics and mechanisms of addiction itself, can easily become traps and distract us from more important goals. These goals should be to identify the main features and mechanisms of addiction and think about the best ways to help addicts. "
As long as scientists agree among themselves, we can extract from their discussion something on which all parties agree: at the heart of dependence is the learning of neurons and neural circuits. And make three practical conclusions: 1) as long as a person continues to use psychoactive substances, the changes underlying the addiction will progress; 2) if you stop using, these processes will stop; 3) the brain is able to learn and change, which means that under conditions of abstinence from psychoactive substances, it will eventually rebuild and adapt to solving other, useful tasks for life. The important thing to understand here is that sobriety is not a goal, but a condition for positive neuroplastic changes.This is the guiding thread. There is no point in singing the praises of sobriety. Sobriety is not an end in itself. But sobriety is an indispensable condition for the activity of the stress systems of the amygdala to return to normal, so that the attraction to psychoactive substances gradually weakened, so that the prefrontal cortex regains its executive functions. Sobriety is a prerequisite to regain yourself and control your life. (But more on that next time.)