
The smallest prosthetics option that allows you to chew a steak at about 75 years old.
Adult children are often unaware that older parents have dental problems. Parents may not share for various reasons and, in our experience, they often try to solve something on their own when it's too late and ineffective. And teeth greatly affect the quality of life of an elderly person and his sense of self. When you can calmly chew food, not feel uncomfortable in conversation (so that your teeth do not fall out) is already good. But many are accustomed to keeping their teeth in a glass, not even knowing that everything can be done much better and more conveniently for a long time. True, of course, not within the framework of the compulsory medical insurance. That is, often they themselves cannot afford this, and they do not want to burden their children. Children, on the other hand, need to know that dental health affects the health of the whole body, and reducing the inflammatory load will greatly facilitate the prognosis of many diseases.
We are accustomed to the good that we have to regularly visit a doctor, and somehow we have already accepted the need to play sports and maintain our health. Unfortunately, this is often difficult to explain to older relatives. As a result, all this leads to a typical sad image of an elderly Russian, which our foreign colleagues call a “Russian bite”: teeth in the chewing section are practically absent, the anterior section has become deformed and parted in a characteristic fan. The importance of hygiene seems to be recognized, but in fact it often turns out that elderly patients do not always know how to properly care for the oral cavity. And they often do not turn to professionals. For them, this is a difficult and not very necessary story. Well, traditional teeth in a glass of water, although it is categorically impossible to store them this way.
I want to talk about relatively minimally invasive implantation techniques for the elderly, which fundamentally change the quality of life. And in general, about what you as children need to know about the teeth of your parents.
Primates, teeth and joints
Our teeth are just the tip of the iceberg. In fact, this is only part of a complex system that includes the chewing muscles, the temporomandibular joint (TMJ), and a very complex built-in system of mechanosensors. Yes, teeth are also an organ of touch, on which a very complex built-in firmware is tied in the form of reflexes that control the movement of the jaw when chewing, swallowing and talking. Have you ever wondered how difficult this process is? The sensitivity threshold of an individual tooth is about 0.8 microns . Therefore, you can easily feel the hair from the soup when you bite it. Its thickness will be approximately 10 times greater: 50–70 µm.
Wise evolution foresaw, or rather, simply killed all other individuals who could not survive the loss of one or more teeth. We are not rodents whose teeth grow all their lives and can potentially grow back if partially lost. The wild primate does not brush its teeth and can only rely on the natural self-cleaning process with tough stems and crunchy fruits like wild carrots with turnips. Sooner or later, caries gets to all teeth, and the dentist has not yet been invented. Chewing is already painful, in the bone tissue there are foci of chronic infection, which crawled through the carious cavity into the pulp chamber of the tooth, and then through the canals went into the area of the apex of the roots. As a result, we became the owners of a fairly flexible built-in program that automatically forces us to chew with the healthy side if the other has bad teeth,cleverly redistributes the load, throwing a new portion of the chewing teeth with the tongue.
Everything is cool, but there are limits. When a primate loses half of its teeth, it most likely dies. Simply because it is not enough to have a healthy and beautiful chewing tooth on the lower jaw. You also need to have a healthy antagonist tooth on the opposite side. Plus, even the coolest incisors won't last long if you try to chew on them. As well as chewing when trying to bite off them. Homo sapiens were a little more fortunate. It is no longer customary to drive out toothless old people out into the cold, but the problems persist. When a person loses their main supporting teeth, the bite becomes non-fixed. To simplify it very much, then all the main anchor points are destroyed, and instead of strict curves when chewing, a person begins to simply click his jaws in an attempt to somehow grind food. Besides,the lower third of the face is reduced and a characteristic toothless profile is formed with sunken lips and a protruding chin. Worse, since the lower jaw has risen higher due to the lack of teeth, the chewing muscles are shortened, and the head of the joints is not displaced correctly.
As a result, we get an unhappy person who cannot chew a banal apple and also suffers from accompanying problems due to deformation of the joints, which are in an unnatural position, and muscle pain due to the incorrect length of the chewing muscles.
What the doctor sees in the elderly
Aging people often find it difficult to look after their apartment, but still refuse conditional help around the house, because they do not want to strain anyone. But the most unpleasant thing is that they often have a similar attitude to their health, in particular, to their teeth.
In a little more detail - about the already mentioned term "Russian bite". This is when the patient has lost the chewing group of teeth relatively early. They are usually lost first due to tooth decay, poor hygiene and poor root canal treatment. In the lateral region, occlusal contacts are lost, and the normal act of chewing turns into attempts to shred food with incisors into relatively swallowed pieces. Further, there is an avalanche growth of problems. As a result, the front teeth, due to the uncharacteristic load for them, first acquire a fan-shaped divergence forward, and then they collapse. This very fan is the Russian bite.
It will not be enough just to take and depict new artificial teeth in place of the old ones. It will take a long time to adapt joints, muscles, rebuild reflexes and a bunch of preparatory procedures.
Sometimes it is necessary to explain in detail that taking care of the oral cavity is no less important than, for example, visiting a cardiologist. We saw both 20 mm dental calculi, which were grown for decades, and the extraction of the roots of teeth, from which droplets of purulent exudate naturally emerged from the infected cavities inside the jaw.
It turns out that your teeth need to be brushed.
As I said, the main problem is underestimating the problem in older patients. The neighbor has been walking without teeth for 20 years, and it's normal. This means that you do not have to worry that the teeth remain less and less. As a result, people are very surprised when you tell them pretty obvious things. You tell them about the importance of brushing your teeth, and you get a surprised expression on your face and phrases like: "Yes, I already have almost nothing to brush." Therefore, it is necessary to remind once again that oral hygiene begins with the first erupted tooth and never ends. A decayed tooth does not hurt, not because it has recovered, but because there is a constant outflow of pus through the canals into the oral cavity. At the same time, the infection does not disappear anywhere and at any moment it can simply kill, provoking phlegmon or other purulent complication.
And also removable structures. My favorite. For some reason, everyone is trying hard to fill them with water and store them in a glass on the nightstand. But in fact, keeping them in water is not worth it at all. Plastics, like acrylic or nylon, absorb water well. Moreover, acrylic is generally porous at the micro level. In water, it is much easier and more comfortable for bacteria to colonize the deep layers of the prosthesis, from where it is difficult to radically etch them. If the denture is poorly cleaned and treated, it turns it into a chronic breeding ground for infection. It all smells very so-so too. Therefore, if you put it in a glass, then only with antiseptics for processing. Although, in general, modern technologies make it possible to completely abandon removable prosthetics in most cases.
What to do with edentulous jaws
The main problem with tooth loss is bone degradation. In our body, everything is quite clear: the load is gone, there is no use - it means that there is no need to spend resources on maintaining bone tissue in the places of the former load.

The jaw of a healthy adult.
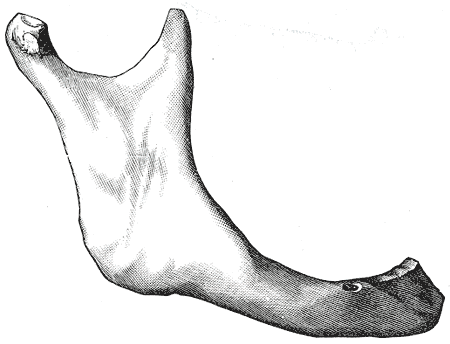
The jaw of an elderly person with complete loss of teeth.
As a result, after years of toothless existence, the loss of bone is so great that nothing remains of the dental alveoli, where the teeth once were. The mucous membrane is also deformed, since the bone base has disappeared.

Upper jaw, bottom view.
The upper jaw has relatively stable bony structures such as the palatine processes of the upper jaw. As a result, this makes it possible to make relatively stable removable dentures on the upper jaw. On the bottom, this almost does not work, if there is not even a part of the preserved teeth. Bone degradation is more pronounced, and in addition there is a movable tongue that constantly throws the prosthesis from its bed.
A thousand devils, piastres, piastres!

Removable dentures are about as comfortable.
Removable dentures are relatively cheap and are often better than nothing at all. But in general, in terms of convenience, they are about the same as Flint's wooden leg against the background of a modern bionic prosthesis. OMS covers only the most primitive options. As in an old joke, when a person handles a nail in his head and specifies how he can be helped with insurance, and he is answered: “Taking out is VHI. And according to the compulsory medical insurance we can only bend! "
Modern research makes it possible to significantly increase the number of cases for implantation. A little higher, I have already given an example of a toothless jaw. If a relatively young patient under 40 years of age lacks bone tissue, then we can "fill up" it. There are special powders based on hydroxyapatite. Some will dissolve, some will assimilate and form new bone, which will enable us to place an implant.
But what to do with patients who are 65+ years old, who in fact are unhappy people with falling false teeth? Circulatory problems and comorbidities do not allow us to add bone tissue that is missing. For this, methods of one-time implantation were created and tested with the installation of some of the implants at an angle uncharacteristic for their teeth. Now I'll tell you more.
No need to let people out into the street without teeth
The most unpleasant stage for any patient is the integration of implants. They don't take root as quickly as many would like. Full integration usually takes two to six months, depending on the jaw, vascular condition, diabetes and the patient's smoking history. Until complete integration with the bone, we cannot transfer the full load to the implants.
We will never let out a person without a temporary construct. You can always choose an aesthetic option so that a person does not have to shine with a toothless jaw in public with the seams of installed implants.
These are all not the cheapest things, and more often than not, older people try in every possible way to show their independence and do not want to depend on children. Therefore, we are sympathetic to the requests of children not to voice the cost of treatment and try to help as much as possible to improve the quality of life of our elderly patients. Well, if you decide to come to us for your own diagnostics or to make a gift to elderly parents - by the word "Habr" a 5% discount.
We had a case when a son approached us about his elderly father. Says: “I know that my father goes somewhere, little by little asks for money for treatment. Can I bring him and you will make an audit? "
My father went to a local professor for treatment with incredible confidence that he was a unique specialist, and only the complexity of his clinical case did not give a good result. As a result, my son and I hardly persuaded him to have a one-time implantation. After all, there is a whole professor, and here a dentist-surgeon, quite young by his standards, offers him some kind of adventure. As a result, we got incredible euphoria when he came to himself after general anesthesia and realized that he was now with teeth. On examination, he looks with the utmost disbelief, feels a tooth and says: “Still in place. Just go crazy, how really it was possible! "
If you still need a removable
We almost never make removable dentures. I have already written that it is extremely difficult to create a normal removable prosthesis on the lower jaw if the loss of bone tissue is great. In traditional methods, there are continuous dances with individual spoons, repeated taking of impressions and fitting, since the prosthesis must be held due to the suction effect on a very mobile mucosa.
Sometimes the patient does not fit the installation of four implants - the minimum required number of supports for non-removable options. Then we can offer the installation of two implants approximately where the canines used to be. On a removable prosthesis, special locks are installed that fix its position relative to the implants. As a result, the chewing load is transferred to the mucous membrane, as before. But the prosthesis itself is stabilized and at least does not move left and right. Then we will think about non-removable structures, but at least the patient will already be able to fully use his removable ones.
What are the options
The more implants you can get, the better usually. The doctor will be able to more evenly distribute the load between functionally different groups of teeth and ensure reliable fixation.
There is such a group of methods of complete prosthetics, when there are no functionally intact teeth on the jaw: “all in N”, where N is the number of supporting implants, usually four or six. Elderly patients often have insufficient bone tissue, and we choose the options that are minimally traumatic for them. It will not work to add bone tissue: it will not take root due to problems with blood vessels and frequent diabetes. Therefore, some of the implants are installed at an angle to the jaw in order to redistribute the load and, roughly speaking, not to drill into the mandibular canal, where the neurovascular bundle goes. All-in-4 is a fairly typical option. This is how it looks. On the x-ray, dark areas are visible near the roots: an infection nests there, which has devoured part of the bone and will shoot at any moment. Well, in general, the clinical situation does not allow saving what is left:
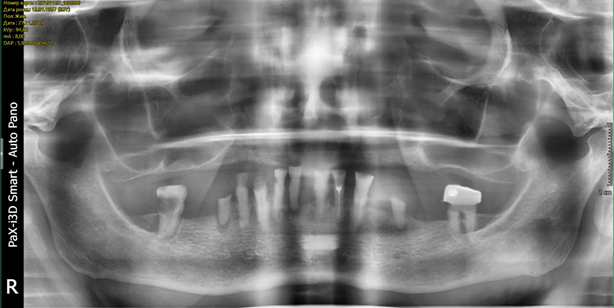

And like this after:


Pay attention to the angle when placing the distal implants.
If we have at least some amount of bone tissue, but not enough teeth, and this happens quite often in old age, then we put six or eight teeth. There is another option when we use a thing called V to V - this is the placement of implants with angulation. The part goes as with all-in-4, that is, two implants - in parallel, two implants - at an angle, and two more implants - at an angle, which are screwed into the distant teeth. This is done when there are at least some of the teeth on the lower jaw or the chewing teeth are more or less preserved. In fact, there are a lot of nuances here.
When not to do all-in-4
The classic all-in-4 is a story about 60+, when you need to provide good aesthetics with minimal trauma and give you the opportunity to eat normally. It is better not to bite off hard sudjuk, but you can eat ordinary food without problems and restrictions. Regular - including steak medium.
If the patient is younger and there are no concomitant diseases, then it is better to install a larger number of implants - all-in-6, all-in-8. The surgeon will have the opportunity to build up bone mass by adding special materials, and the patient's healthier vessels will allow osteocytes to settle there with minimal resorption of the material. Therefore, patients under the age of 40 are almost certainly better off not using four-implant techniques. Six implants can almost always be placed on the lower jaw if there is no pronounced degradation of bone tissue due to prolonged absence of teeth and aggressive periodontitis.
It usually makes sense to use zirconium dioxide as a framework for a fixed prosthesis. You most likely met this material in the form of a ceramic knife blade. It is very hard, lightweight and white in color. Why is it better than traditional cobalt chrome steel or titanium for example? Metal has very poor adhesion to ceramics. It is very difficult for the technician to ensure high-quality adhesion of the ceramic mass on the metal. We have to create mechanical roughness and other tricks before baking the ceramics in the oven. In the case of zirconium oxide, the adhesion is extremely high even without the use of special adhesives. And also zirconium does not give a translucent cyanotic-metallic shade to ceramic teeth, which is characteristic of almost any cermet, except, perhaps, gold.

This is what the navigation template looks like. It is printed from special polymers on photolithographic 3D printers. All design options are based solely on navigation templates. Modern protocols do not imply screwing the implant "by eye" at all. You must first plan the position of the implant in the bone on the model obtained from cone beam tomography, and then make a template on a photopolymer printer. You simply apply the template to the jaw and enter the cutter at a pre-calculated angle to a strictly specified depth. In this way, we precisely ensure that the implant will be in the pre-planned place and at the right angle.
If you're interested, here are some videos about the manufacturing process:
Here is a video
Please note that all-in-4 and all-in-6 are technologies slightly discredited due to aggressive marketing and the constant expansion of indications for installation. It is not a panacea, it is not a solution to all jaw problems, and in many cases by the age of 45 or so, other methods must be used for medical reasons. Nevertheless, it is the correct application of such implantation without expanding the indications in old age that often makes it possible to replace uncomfortable prostheses with almost normal teeth.
A little about dementia
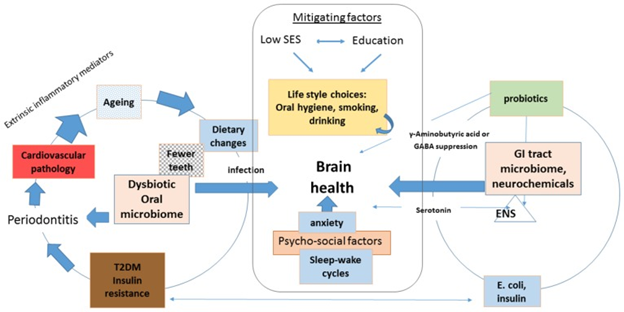
The relationship between periodontitis and early dementia. Link.
Unfortunately, many people think that dental problems are not particularly critical. As a last resort, there is always a blender. In fact, problems in the oral cavity can lead to a very complex chain of consequences. Thus, several studies suggest a correlation between early dementia, Alzheimer's disease and chronic periodontitis. In the first, they simply found a similar connection, and in the second , the assumption has already been expressed and partially proven that this may be due to a violation of the microbiome, which leads to chronic inflammatory processes not only in the oral cavity, but throughout the entire gastrointestinal tract, including the intestines.
Therefore, I would highly advise you to devote more time to prevention, so as not to reach the costly and complex methods of treatment. And elderly parents definitely should not be left alone with their problems, even if they are modestly silent about them.