Millions of hearts stop every year. Why can't we replace them?

The heart from Bivacor contains a titanium chamber with a rotor that rotates in the center and sends blood into the body.
Daniel Timms began working on his artificial heart in 2001 when he was twenty-two years old. He was a biomedical engineering graduate student and lived with his parents in Brisbane, Australia. He was looking for a topic for his dissertation when his 50-year-old father, Gary, suffered a severe heart attack. At first, the doctors thought it was a valve, but later it turned out that the man had problems with his whole heart. Heart failure is a progressive disease, and a person can live for years while their heart breaks down. There was little time. The topic for research appeared by itself.
Gary was a plumber and Daniel's mother, Karen, was a high school lab technician. Their family was often engaged in experiments. As children, Daniel and his father constantly built intricate systems of fountains, ponds and waterfalls in their backyard. It is not surprising that now they are together to work on the heart. They bought hoses, pipes and valves from a hardware store and built a rough model of the circulatory system from them. Timms began researching the history of artificial hearts. The first human implantation was done in 1969 by a surgeon named Denton Cooley of the Texas Heart Institute in Houston. The patient, Haskell Karp, was treated for sixty-four hours - a great success considering that his heart was excised from his chest. The engineers were confident that the problem would be solved in a few years.
One of the first prototypes of the 60s of an artificial heart from the engineer Willem Colf .
However, many problems arose. It was difficult to develop a small device capable of beating thirty-five million times a year, pumping 9,000 liters of blood a day for many years. In the decades that followed, patients could live days, months, and even years with various artificial heart patterns, but their quality of life was often poor. They were connected by pipes to large machines; they often suffered from strokes and infections; their new hearts were too big or had parts that wore out. Every year, millions of people around the world die from heart disease, while only a few thousand hearts were available for transplantation. As Timms found out, existing solutions can only give people the opportunity to "wait" for artificial hearts that may never appear.A permanent artificial heart has never existed.
Studying the projects, Timms found that many of them were developed in the 60s, 70s and 80s, he believed that it would be easy to significantly improve them. Previously, most artificial hearts were made from flexible plastic: he could have made it from durable titanium. Pumps were typically pneumatically driven, with air pushed through tubes - Timms could use an electromagnetic drive to do this. Most importantly, if traditional artificial hearts "pulsed" (they rhythmically squeezed blood out of the artificial ventricles), then in Timms' device it would move in a continuous flow. Timms made a rough sketch on paper. The blood flowed into a small chamber with a rotating metal disc in the center. The disc, like a propeller, pushed the blood out - into the lungs and other parts of the body. It was a smart and economical design,who did not imitate the natural heart, but rethought it. Under the sketch, Timms wrote "damn it, yes!"
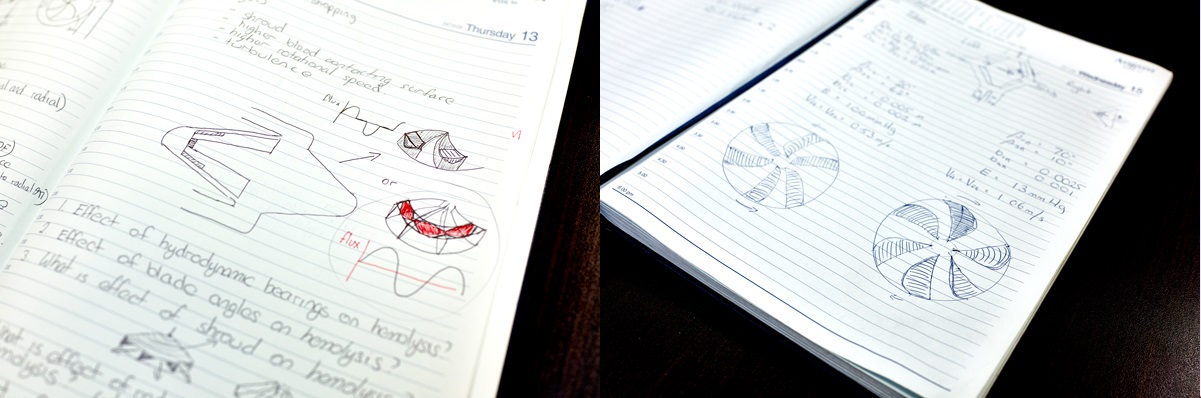
Daniel and his father made a prototype in the garage. It was made of clear plastic and successfully distilled water through a simulated circulatory system in which tiny balls represented blood cells. But there was a problem - in the place under the rotating disc, the flows stopped and the balls got stuck. This funnel is very dangerous: the blood cells that clump together tend to coagulate, creating clots that can cause strokes. On Skype, Timms spoke to a researcher in Japan who was working on magnetic levitation systems used in high-speed trains. They decided that stronger magnets could be used so that the disc could be suspended further away from the walls of the heart so that blood could flow more easily around it.This “magnetic levitation” approach also solves the problem of wear and tear - no part will come into contact with another.
Timms was still a graduate student when he made an appointment with cardiologists at the Brisbane hospital where his father was being treated. He pulled a plastic pump out of his backpack and explained how the heart would work, based on his design. One doctor left the meeting incredulously. Another provided Timms with a small allowance and a room in the basement. In 2004, while Gary was recovering from upstairs valve replacement surgery, Timms worked on prototypes downstairs. Soon, his artificial heart was able to extend the life of a sheep for a couple of hours. Like engineers from the past, he expected further progress to be rapid.

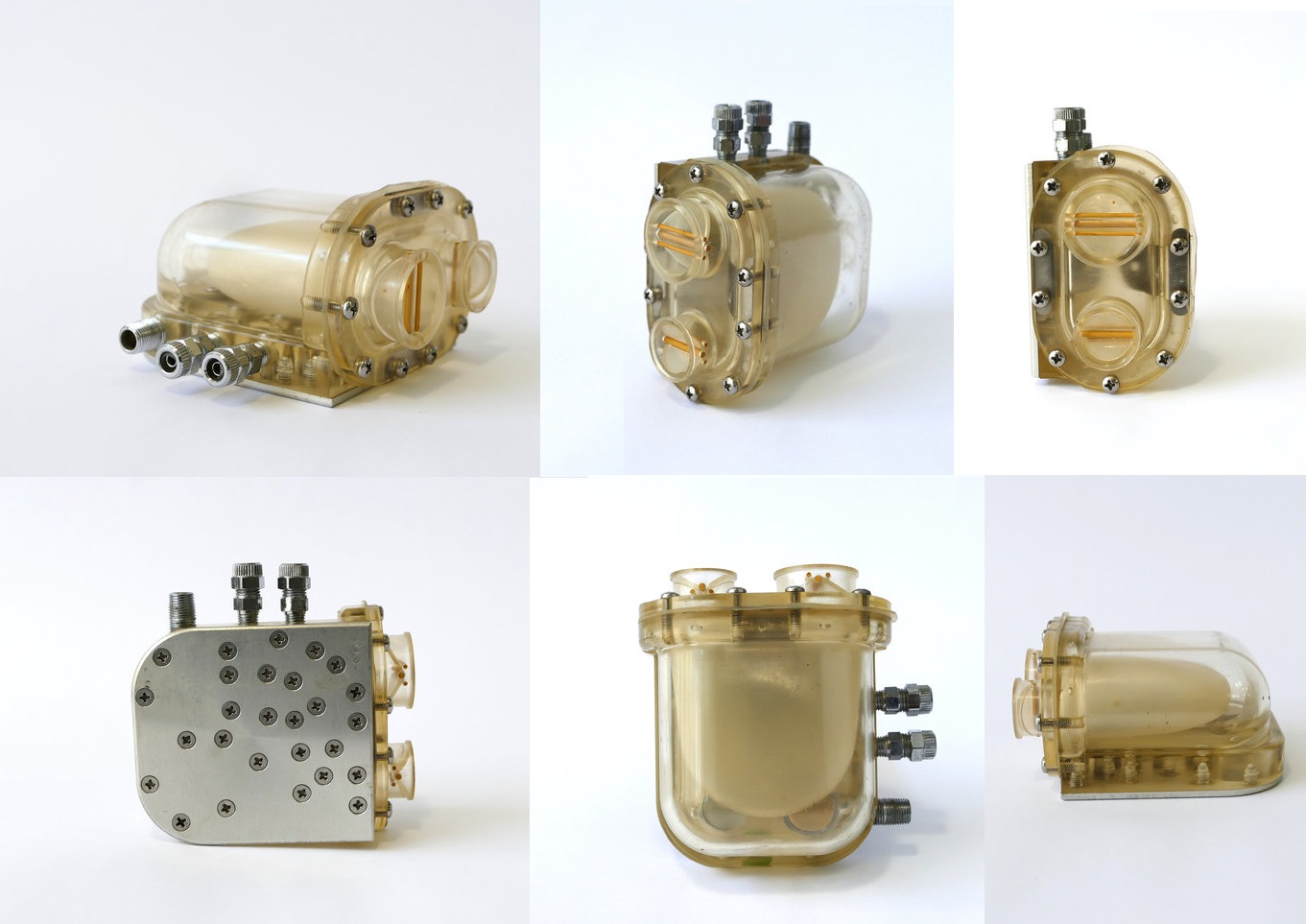
Today, more than a decade and a half later, Timms' company Bivacor is based in Cerritos, a Los Angeles suburb. About a dozen engineers work in a building surrounded by palm trees and flowering hedges. Last year, before the pandemic, Wilson Xe, a twenty-three-year-old biomechanical engineer, stood over a laboratory table and wielded ties to attach the latest version of the heart from Bivacor to a model of the circulatory system. The system, known as the "loop," has been vastly improved over the one that Timms and his father built. Made of plastic tubing and a little over a meter high, it resembled a model of a roller coaster. The system was filled with water mixed with sugar to simulate the viscosity of human blood. It also used valves to simulate different circulatory conditions: high and low pressure,stagnation and fast ducts. The heart attached to the system was sturdy and crafted in steampunk black and gold titanium. Four openings led to the aorta, vena cava, pulmonary artery, and pulmonary vein; a cable connected it to a control unit the size of a dictionary. This cable will pass through the skin in the abdomen and people will need to carry the control unit with them at all times.
When Xe adjusted the circuit valves, air was pumped out with a hissing sound. Nicholas Greatrex, an Australian electrical engineer, entered a command on a computer, and a current began to flow to the electromagnets of the heart. Water ran down the loop, moving with a low throbbing hum.
The Bivacor heart and the human heart work on different principles. The human heart has two sides. Blood first flows from the smaller, right side to the lungs and back, being saturated with oxygen. It then moves to the larger, more powerful left side, pumping blood into the body. The heart from Bivacor is based on a combination chamber. It sends blood in two directions through a rotating disc ("rotor") that has two differently shaped sides (to create the required level of blood pressure). If the heart of a healthy adult beats anywhere from sixty to one hundred times a minute, the Bivacor heart spins at 1600 to 2400 rpm.
Measure the pulse of a person using such a heart, and you find only constant pressure - like in a garden hose. Some heart surgeons and cardiologists don't like the idea of a heart without a pulse. Tapping on a computer keyboard, Greatrex ordered the rotor to run at variable speed. “By accelerating and decelerating the rotor, we can create an artificial pulse,” he said. I reached out and touched one of the loop's white rubber hoses. Oddly enough, he was warm; under my fingers, it began to throb in a familiar human rhythm.
Blood pressure 100 to 70, Greatrex said triumphantly, touching his wrist. “The doctor can look at this and say:“ You are doing well! ” According to the Centers for Disease Control and Prevention, approximately 6.2 million Americans suffer from some form of heart failure, often experiencing weakness, shortness of breath, and instability. Such an artificial heart will turn back time.
Bivacor is in a transition phase. The company has yet to sell its products and is completely dependent on venture capital funds, business angels and government grants. Her hearts were implanted in sheep and calves - they lived for months and sometimes ran on a treadmill. The company is preparing to file an application with the Food and Drug Administration (FDA) for approval for human implantation. Crossing the threshold between animals and humans means entering a tough regulatory environment. In the early days of artificial heart research, the team could implant a device in a dying person on an emergency basis - as a last resort to save his life - and see how it functions.
Ethicists were concerned, but progress has been rapid. Today, such experiments are prohibited: the design of the heart must be fixed and approved before the start of clinical trials; the trials can take years, and if the heart is found to be not good enough, the process must start over. Bivacor is currently deciding which features will be included in their heart's clinical trials. The wrong decision will most likely lead to the loss of the company. There will almost certainly not be a second attempt to climb the summit.
Timms, short-haired and red-haired, is now forty-two. Since his time in Brisbane, he devoted almost his entire working life to heart work, traveling to Japan, Germany, Taiwan and Houston to work with various surgeons and engineers. Quiet and focused, he is very restrained: he prefers not to tell people what he does for a living, so that the subsequent conversation does not tempt him to advertise a project whose deadlines have long been disrupted. Wearing jeans, trainers and a crumpled dress shirt unbuttoned to the third button, he led me into a back room where half a dozen heart prototypes worked continuously for sixteen months. “It's very important to show that they never, never stop,” he said through the hum of the moving water. Timms himself looked like he hadn't slept properly for a couple of decades.
On our way out of the lab, we walked through a conference room where the engineer videotaped how to test a heart from Bivacor before implantation: “Place your thumb on the left inlet and press lightly,” she said. The furniture in Timms' office could be in his home study (it was a gift from one of the first investors - the owner of a furniture store in Houston). There was an ironed shirt on a hanger on the wall, and a road bike in the corner.
Sitting in his creaky chair, Timms remembered driving his father to the hospital in 2006. The valve replacement surgery helped Gary restore his heart function, but only temporarily. “He has a blood clot on a mechanical valve,” Timms said. "It kept blood flowing to the left side of his heart and lungs." Timms depicted the accumulation of growths with his hands, showing a path from the left side of the chest to the sternum and up the neck - blood accumulated like water, struggling to drain out of the sewer. “This causes swelling,” he said. "Blood coughs up because it passes through the lung membrane."
Two weeks later, Timms was in Germany, meeting with pump engineers, where he learned that his father was getting worse. He immediately flew home, but did not have time to talk to his father for the last time. “He was in intensive care with tracheal ventilation and everything,” Timms said. "His death only strengthened my resolve." I thought, “That's it. We will do it at any cost. "
I asked Timms if, two decades ago, he really believed he could invent an artificial heart in time to save his father.
He swayed back and forth, nodding. “If at that stage there was a device that could be implanted in him, then perhaps he could stay for another five or ten years - he would see how I got married and how I had children. He could have lived through it with us. Then philosophy was this. Five or ten more years. " He laughed. “It never happened,” he said, referring to marriage and children. He gestured around the office. "I'm stuck in all this."
Before the heart was replaceable, it was inviolable - the forbidden frontier of surgery. Nineteenth century physicians believed that the heart was "the limit set by nature." In the first half of the twentieth century, anesthesia made surgeons bolder. They began to intervene to heal the arteries and valves while the heart was still beating. They tried to cool patients down to hypothermic levels and then quickly act on their heart until it was beating. It wasn't until the 1950s, with the development of the heart-lung machine, that open-heart surgery became commonplace. Blood exits the body and into the machine, bypassing the heart and lungs, and gives surgeons access to an immobile and bloodless heart that they can treat almost like a normal muscle.
Early heart-lung machines were the size of a desk and could only be used safely for short intervals; however, they made the artificial heart desirable and possible. The same goes for several other trends. More people lived to be sixty and seventy, when heart disease statistics began to deteriorate: by mid-century, 40% of deaths in America were due to heart disease. These statistics have raised serious concerns among policymakers. In 1948, Congress (a group of aging men) passed the National Heart Act, beginning a decade of expansion in federal funding for cardiac research.
It was the era of Apollo, and the artificial heart seemed like a breakthrough. In 1964, the National Institutes of Health launched the Artificial Heart Development Program, a multi-million dollar engineering project to begin implanting hearts in patients by the end of the decade. In structure, it was similar to the NASA project. He provided grants and contracts to teams of engineers who competed to design the best valve, pump, or power supply; several teams have experimented unsuccessfully with nuclear-powered hearts. Time and Life magazines have dedicated their covers to this topic. As medical historian Shelley McKellar writes in her book Artificial Hearts: The Allure and Ambivalence of a Controversial Medical Technology, high hopes for artificial organ implants "do not necessarily reflect current surgical reality."
The true complexity of the task quickly became apparent. At Maimonides Hospital in Brooklyn, Adrian Kantrovitz, an inventor surgeon who helped improve the pacemaker and heart-lung machine, began working on the pump. He took a sensible approach: instead of replacing his heart, he installed a pump right behind him to compensate for his weakness and perhaps give him time to recover. Kantrovitz's prototype pumps were tested on dogs and by 1966 he was ready to implant them in humans. The first human patient to receive such a pump died after severe bleeding. The second was a 63-year-old bedridden and diabetic woman who had two heart attacks - she lived for twelve days, but died after a series of strokes.
When Kantrowitz pulled out his pump and opened it, he found clots. He faced an obstacle that later became known as "hemocompatibility". Too much force or pressure can rupture blood cells. They can be soldered in funnels and crevices. They can adhere to textured surfaces. Kantrovitz devices changed the structure of the pumped blood, and as such "distortions" accumulated, the consequences worsened.
Meanwhile, at Baylor College of Medicine in Houston, Michael DeBakey and Denton Cooley, who were considered the best cardiac surgeons in the world, tackled a different set of challenges. DeBakey and Cooley started out as partners - they performed a huge number of heart surgeries at an incredible pace. As he writes in his book Ticker: The Quest to Create an Artificial Heart by journalist Mimi Schwartz, later the two fell out. Cooley left the practice in 1960 and later founded the Texas Heart Institute. Meanwhile, DeBakey hired Domingo Liotta, an innovative Argentine heart surgeon, to work with the artificial heart. By 1969, Liotta began implanting prototypes in calves. The results were discouraging (of the seven animals, four died on the operating table), and DeBakey thought they were not yet ready for use in humans. But Cooley was keen to move the work forward. He had patients awaiting a donor heart - not only at his hospital, but also in nearby motels. Without informing DeBakey, he hired Liotta to work at the Texas Heart Institute with the expectation of using a new implant.
Cooley began looking for a candidate among his patients. Haskell Karp, a 47-year-old appraiser from Skokie, Illinois, has been hospitalized thirteen times due to heart disease. He had such severe shortness of breath that it was sometimes difficult for him to comb his hair. Cooley wanted to see if Karp's heart could be surgically repaired, but Karp and his wife agreed that if there was no such option, Cooley could implant a prototype Liotta in the hopes that a donor heart would later emerge. “Mr. Karp was taken to the surgical ward,” Cooley later wrote in his memoirs. “He was pale, sweating and breathing hard. His blood pressure dropped to half the normal level. " Halfway through the operation, it became apparent that his heart could not be saved.
Cooley set up a pneumatic device connected by hoses running through Karp's side to a console the size of a refrigerator. The ventricles of the heart were made of elastic plastic with a flexible polyester lining; when air passed between the mucous membrane and the plastic, the ventricles contracted and the heart worked. The device kept Karp alive for sixty-four hours until it was replaced by the transplanted heart of Barbara Evan, a forty-year-old mother of three. However, thirty-two hours later, Karp died of pneumonia and kidney failure, the aftermath of a serious heart condition that initially made him a candidate for the risky procedure. Cooley regarded the operation as a success. But DeBakey, enraged at stealing his artificial heart, doubted that his former partner was acting ethically. A number of investigations have been carried out,and Cooley denounced the American College of Surgeons. Observers disagreed as to whether the operation was heroic or reckless, but in any case, a new problem arose: by the time people agreed to an artificial heart, they were so sick that it was almost impossible to save them.
Willem Kolff, the Dutch-born therapist who invented dialysis in the 1940s, didn't stop that. He didn't just want to get as close to transplantation as possible, he wanted to create a heart so good that it could be used to work on a permanent basis. In Colff's laboratory at the University of Utah, an engineer named Clifford Quan-Gett created a soft ventricle that did not damage the structure of the blood. Robert Jarvik, a talented biomedical engineer who joined the University of Utah team during his medical school, has tirelessly refined the design and manufacturing process to address hemocompatibility issues. When Jarvik joined the team in 1971, their heart prototype could keep a calf alive for just ten days. However, the progress was steady - after ten years of work,a calf named Alfred Lord Tennyson lived for two hundred and sixty-eight days on what was by then called the artificial heart of Jarvik-5.

In December 1982, heart surgeon William De Vries implanted an upgraded version of the heart (Jarvik-7) on Barney Clark, a sixty-year-old dentist. Clark's heart worked for about a sixth of its resource. He felt so bad that when he saw the calves and sheep with Jarvik's hearts, he said, "I think they feel much better than I do now." The operation attracted international attention. Often the focus was on the personalities of the participants: De Vries, the experienced and "Lincoln", Jarvik, the young and handsome, and Clark, a charismatic man in the street who performed combat missions during the Second World War. A video of the seven and a half hours of the operation was broadcast on television. Afterwards, reporters attended the daily press briefings held in the university cafeteria.
Clark lived one hundred and twelve days with pipes connecting him to a four-hundred-pound pump and control panel. He was in periods of decline, then recovering, then was unhappy, then optimistic. Sometimes he even stood briefly and pedaled the stationary bike, but usually he lay in bed and gasped, drawing air through the mask. One of its mechanical valves had to be replaced in a subsequent operation. Clark suffered from nosebleeds, seizures, kidney failure, and pneumonia. Shortly before he died of sepsis and organ failure, he said, interrupting the puffing sound of the air pump, "It was nice to be able to help people."
The FDA gave De Vries permission to implant seven artificial hearts, and he got down to business. In 1984, De Vries installed a modified version of the Jarvik-7 to William Schroeder, a 52-year-old army ex-weapons inspector. Before the operation, Schroeder asked to confess. In the end, he lived for 620 days, moved from the hospital to an apartment, and from time to time used a portable pumping unit, which ran for three hours on battery power, to go out into the corridor or drive a car with his son. In a telephone conversation with Ronald Reagan, Schroeder jokingly complained about the delay in social security checks. Feeling the man's chest, the reporters marveled at his heartbeat - it seemed more powerful than that of a healthy person. However, Schroeder suffered from a variety of ailments. In particular, from strokes - one of them was extensive. After,As he died of chronic infections and lung problems, he was buried with a tombstone depicting two hearts - a human and Jarvik-7.
Hearts got better, as did surgical techniques, although none of these improvements changed the mainstream of research. De Vries made several more transplants, with varying success. In Sweden, the man who was presented with the Jarvik-7 felt very well, went for long walks and ate at his favorite restaurants. However, he died seven and a half months later, sparking a legal debate about whether he was even alive (according to Swedish law at the time, he died the moment his heart stopped). Doctors, patients, and reporters began to feel cooler about the topic. Confidence in the idea of a heart replacement began to fadeand sponsors wondered - wouldn't it be better to spend money on something else? What is the point of short term artificial heart transplant? Did the surgeons try to save their patients or were they just experimenting with them? Was the added days worth it?
The early artificial engineers had limited success. Their devices could keep patients alive for a long time, but not permanently. Heart failure was no longer fatal, but the quality of life was too low. A limited miracle, an ambiguous good. “They did it,” Timms said in his office as we discussed the story. "However, no one wanted that." A sobering conclusion for those who tried to repeat.
A couple of decades ago, at the beginning of my last year of college, I found myself living next to two charming women: Seuss from Montana and Jess from New Jersey. We became friends and I soon learned Jess's story. In high school senior, she suffered a massive heart attack. After the last rites, she was saved by implanting an experimental heart pump - a "ventricular assistive device" called the HeartMate. This device was the heir to the inventions of Kantrowitz from the 60s, but it was not an artificial heart. HeartMate performed the functions of the right side of the heart, the left remained in place. Jess attended the prom and starred in the school's production of Effortless Business Success, while connected via a wire to a battery in her purse.She learned to walk with a prosthesis because a complication from a heart attack required the amputation of her left leg above the knee. A few days before graduating from high school, she received the heart of a teenage girl who died in a car accident. Shortly thereafter, she developed non-Hodgkin's lymphoma, likely as a result of the immunosuppressants she was taking to prevent rejection. When I met Jess, it was all over. She didn't have a battery, she was cured of cancer, and she was getting higher education.as a result of the immunosuppressants she was taking to prevent rejection. When I met Jess, it was all over. She didn't have a battery, she was cured of cancer, and she was getting higher education.as a result of the immunosuppressants she was taking to prevent rejection. When I met Jess, it was all over. She didn't have a battery, she was cured of cancer, and she was getting higher education.
We remained friends after college. Jess has worked in the healthcare industry as an organ donation attorney. Her special feature was that she knew how to be sweet and tough at the same time. She traveled the world, beat cancer twice, went to concerts, ate a lot of desserts, had boyfriends, and got promotions. In general, she behaved like an ordinary young girl, and not like a living miracle. Observing the ease with which she moved in any medical facility - communicating with nurses, sending emails from her hospital bed - I realized how thoughtful and courageous she lived.
Curious to meet the people behind HeartMate, I drove to the Texas Heart Institute in Houston. It is located near St. Luke's Hospital, in the city-like Texas Medical Center, the world's largest medical complex, with ten million patients a year. This is Vatican Cardiology. There is a large museum dedicated to the history of heart surgery and heart pumps. Not far from where Denton Cooley implanted the first artificial heart more than five decades ago, I sat in a windowless conference room with two surgeons, O. H. (Bad) Fraser and Billy Cohn. Kon, a tense man in a black button-down shirt and jeans, was fifty-nine; Fraser, a man of few words in a blazer, trousers and tortoiseshell-colored glasses, was seventy-nine. Both of them were wearing cowboy boots.Together they have implanted more than a thousand devices for "mechanical support of blood circulation". Most patients today are fitted with ventricular assistive devices to help or replace the left side of the heart. But Cohn and Fraser, like Timms, are part of a small group of researchers still working to create a complete and permanent heart replacement. In 2011, they implanted two HeartMate IIs (one for the left side, one for the right) in a fifty-five-year-old man whose heart had completely failed and was removed. These devices acted like an artificial heart and allowed the man to live for 5 weeks.that help the left side of the heart or replace it. But Cohn and Fraser, like Timms, are part of a small group of researchers still working to create a complete and permanent heart replacement. In 2011, they implanted two HeartMate IIs (one for the left side, one for the right) in a fifty-five-year-old man whose heart had completely failed and was removed. These devices acted like an artificial heart and allowed the man to live for 5 weeks.that help the left side of the heart or replace it. But Cohn and Fraser, like Timms, are part of a small group of researchers still working to create a complete and permanent heart replacement. In 2011, they implanted two HeartMate IIs (one for the left side, one for the right) in a fifty-five-year-old man whose heart had completely failed and was removed. These devices acted like an artificial heart and allowed the man to live for 5 weeks.These devices acted like an artificial heart and allowed the man to live for 5 weeks.These devices acted like an artificial heart and allowed the man to live for 5 weeks.
Fraser's career began in the golden age of artificial heart work and continued into its darkest years. In 1963 he entered Baylor College of Medicine and studied with Michael DeBakey. He joined Cooley's team in Texas in the 70s and worked there in the 80s, when the discovery of cyclosporine and immunosuppressive drugs improved transplant survival. Convinced of the importance of heart pumps as intermediary devices, he began working in a basement laboratory where pigs, sheep, cows and goats were kept. For decades, he collaborated with engineers to test and improve nearly every heart pump in existence today, including the original HeartMate. (Earlier in Cerritos, I watched a video of a calf with a Bivacor pump walking on a treadmill in Fraser's lab. Fraser and Cohn are consultants for the company.)
“This guy, O. H. Fraser,” Cohn said, pointing to a photograph of Fraser in a blood-stained robe taken a long time ago on his laptop. "A real rock star." Fraser chuckled.
Cohn, who radiated messianic energy, said that in 1986, Fraser was the first surgeon to successfully use HeartMate in clinical trials that took place prior to 1993. Since this device was approved by the FDA, it has been installed in approximately 4,000 patients. HeartMate was donut-shaped, equipped with a mechanical pump and one of its main innovations was the use of specially textured plastic and titanium on which blood cells could form a smooth biological surface. Early versions were powered by air delivered through a hose. Later models, such as the one Jess received, had a motor. The device's lifespan was no more than a year and a half, but that was enough for patients who were hospitalized with blue lips and were close to death."You had to put the HeartMate in the breathing apparatus, make a large incision, insert the pump into the abdomen, plug it in, and at the end of the operation the lips turned pink." The problem was and remains the absence of transplanted hearts: "In a year and a half HeartMate will break, and you had better find a donor heart during this time, otherwise these people will die."
To address this issue, Fraser partnered with Abiomed, a Massachusetts heart pump company, to create the next generation artificial heart, AbioCor. This artificial heart was created in the early nineties. It was traditional in some respects (it has two chambers, like a real heart), but otherwise it is a very futuristic device. No air hoses or electrical cables came out of the body. The AbioCor is a completely self-contained implant that uses circulating hydraulic fluid to compress the ventricles. The AbioCor is powered by a battery that can be charged wirelessly through the skin. In theory, you can swim with it.
“Super, super ambitious,” Cohn said as he opened the chart. “They spent a quarter of a billion dollars on this. Several hundred animals, and half of the operations Bud and his team have done here. " In 2001 and 2002, hearts were installed in 14 patients. It was then that ambitious plans began to crumble. “After 9 months, all but four died of complications or device failure,” Cohn recalls.
The FDA gave Abiomed permission to implant 60 more devices, but it was clear to everyone that they needed to be updated and then approved again - a lengthy process that no one had the heart to tackle. “The Abiomed gave up,” Cohn said. "They said, 'This is too difficult!' The problem was that the heart was so large that it could only fit in the ribcages of the largest male patients.
“You know, your heart beats a hundred thousand times a day,” Fraser drawled.
“Thirty-five million times a year,” Cohn said.
“Given this fact, it's amazing that it lasted so long,” Fraser said.
Throughout the eighties and nineties, even as he worked on HeartMate and AbioCor, Fraser argued that engineers should move from pulsating pump designs to designs based on the simpler mechanical principle of "continuous flow" - which is what Bivacor is based on. Some researchers have argued that the cardiovascular system can benefit from the pulse: there is evidence that the walls of blood vessels dilate in response to a rapid heartbeat. But Fraser concluded that for all the benefits of pulsation, they were outweighed by strength and simplicity. He began working on two continuous flow projects in parallel, one with cardiologist Richard Wempler, and the other with Robert Jarvik. They implanted artificial hearts in animals and then removed,disassembled and analyzed how they work. By the two thousandth, these devices went into operation under the names Jarvik 2000 and HeartMate II, respectively.

Cohn opened up the HeartMate II circuit on his laptop. Basically, it is a narrow tube with a corkscrew. When the screw rotates between the two bearings, it acts like a stationary propeller, continuously pushing blood from the heart into the aorta above it. (In agriculture, the same design is called the Archimedes screw and is used to pump water)
Cohn pointed to the propeller: “Here is a moving part suspended from ruby bearings. People said, "You can't use bearings in the blood." It turned out that you can! There is enough blood going through them to keep them clean. " Clots are still a problem, as are infections. However, more than a thousand people each year receive and live with HeartMate II or similar devices as they move up the transplant waiting lists. HeartMate II kept Dick Cheney alive from 2010 to 2012 until he got a transplant.
In the summer of 2019, I received a message from Jess. “I recently celebrated the 20th anniversary of my heart transplant,” she wrote. "But a transplanted heart does not work as long as a native one." I did not know that. I assumed her transplant was permanent. In fact, her borrowed heart was breaking down. She gasped and nearly fainted one night as she walked home to her apartment. Now she has returned to the hospital awaiting a second heart. “It could be weeks, months, or (less likely) it will be transplanted tomorrow,” she wrote. "Please send something nice."
I visited Jess in the ICU where we talked about restaurants, careers, and TV shows. We looked at some pictures of my son, who was about a year old. I was about to visit again when she died.
“She did a great job,” Cohn said. "Many heart transplant patients die after ten years."
“I was recently at a birthday party for a guy who had a transplant thirty years ago,” Fraser said. “But this happens very, very, very rarely. Only about 5% of heart transplant patients live another 30 years. ” Artificial pumps on the market are considered bridge therapy, and heart transplants are “targeted” therapy. However, if you live long enough, grafts will also be just bridges.
I asked Fraser and Cohn what they thought of all the people who died during or after using their devices - whether they lingered in this world and how they lived.
“Martyrs,” Cohn said. “They clung to life. The technology might not have been there, but it probably put off their last breath. Many of them spent years with their loved ones, doing what they liked. Some went to the intensive care unit, spent six weeks there, and died. In hindsight, sometimes it seems like it was better to just let them go. But you never know! This is a game with statistics, and they were ready for it for another couple of days of life. And every time it helped us move forward. "
“I worked a lot with children with leukemia when I was a student,” said Fraser. “They all died. The doctors in the Texas Children's Department wanted to quit their jobs. "
“This is because you tortured them with these poisons,” Kohn noted.
“They looked terrible,” said Fraser. “Their bellies were swollen, they were losing hair, it scared other children. But the doctors continued to do all this. I think it helped me in the future, because the first 22 people out of 70, whom we installed the first artificial ventricles, died. "
It was too late. Fraser led me through a deserted office, through winding, quiet corridors, and finally we took the elevator down to the basement. We entered his laboratory, a huge den where he spent most of his working life. We went through the veterinary operating room and pathology laboratory, where dead animals and failed pumps could be disassembled and analyzed.
“We've got pigs here,” Fraser said as he opened the door. It smelled like animals, and a large, pink, snoring pig appeared in sight.
“Pigs have the most human heart,” he said, closing the door. He pointed into the corridor: “Goats. I don't like working with goats. They are too smart! " He laughed. "They're looking at you."
We went deeper into the laboratory. In a carpeted conference room, several dozen artificial hearts and heart pumps lay on display — almost a museum for the entire area. “What's in the middle is AbioCor,” Fraser said, pointing to a twisted piece of metal and plastic in the shape of a heart. "This is old Jarvik-7": two yellow-beige ventricles with outgoing tubes. “This is HeartMate II”: a gray metal cylinder with white tubes at both ends that looks like something you'd find under a sink. The September 1981 cover of Life magazine read, "Artificial Heart Created" in a frame on the wall.
Fraser pointed to a large metal pump and a white tube protruding from it — a “long tube,” he said. Until it was replaced, the device was doomed to fail. Small changes are made iteratively, and their effects are revealed only after death. It was an invention in slow motion.
The AbioCor project has been canceled. The work on Bivacor is still many years away. Today, the only company that manufactures and markets artificial hearts that are implanted in humans is SynCardia Systems in Tucson, Arizona. The company was established as part of a rescue mission. Symbion, the Utah company that Robert Jarvik helped found, lost its Jarvik 7 certification in 1990 due to quality control issues. The technology was bought out by another firm conducting clinical trials with an improved version of the device, but it ran out of funding in 2001. For a while, it seemed that technology would simply disappear. But two cardiac surgeons and a bioengineer have together amassed venture capital to buy out the rights to the system. They renamed the device to SynCardia Total Artificial Heart, or TAH Company.which is now based in several buildings surrounding a sandy car park, sells about a hundred hearts a year, all descended from the old Jarvik 7, which was powered by air. Despite the fact that SynCardia has managed to create a team of surgeons capable of establishing the company's hearts, it performs very poorly. The company recently passed Chapter 11 of the Bankruptcy Code and was bought out by new investors. They dealt with the pandemic that led to the cancellation of operations across the country through the production and sale of hand sanitizer.The company recently passed Chapter 11 of the Bankruptcy Code and was bought out by new investors. They coped with the pandemic that led to the cancellation of operations across the country through the production and sale of hand sanitizer.The company recently passed Chapter 11 of the Bankruptcy Code and was bought out by new investors. They dealt with the pandemic that led to the cancellation of operations across the country through the production and sale of hand sanitizer.
Together with Karen Stamm, program director at SynCardia, and engineer Matt Schuster, I watched through the window as a technician in a clean room collected one of the hearts. “The key to creating an artificial heart is the material we use,” Schuster said. “Segmented polyurethane mortar. We call it "spazz" - from SPUS. " The strain laughed. “We make this stuff here on campus,” Schuster continued. “This is our own proprietary blend. When it comes out of the production equipment, it looks like juice or thick honey. " Using a toothpick, the technician carefully applied layers of molded honey. A translucent something appeared on top of another translucent something. The assembly process takes two and a half weeks.
We went through a lab dedicated to explant analysis. “If we get the heart back, we take it apart and examine it,” Schuster said. We found ourselves in another room filled with several dozen water tanks on the shelves. A heart beat inside each reservoir. Next to the tanks were air pumps, or "drives". The sound in the room was deafening, fast and loud: bang, bang, bang, and inside it you could hear the mechanical clatter of a typewriter. The sounds were repeated twice a second - in the rhythm of production, as if we were in a factory. “This is where we do our long-term research,” Strain shouted over the noise. On the one hand, there were hearts of 50 cubic centimeters (they are placed in small patients), and on the other - 70 (they are placed in larger patients). “Here are the drives,from which there is a mechanical sound, ”said Strain, pointing to a mechanical pump that looked like a lunchbox. It was connected by an air tube to the heart inside the reservoir. "When you hear a click, a valve inside the heart is firing."
The main innovations of SynCardia were directed precisely at the drive. Their heart can be powered by one of two devices: the first is the size of a mini-refrigerator, and the second is the size of a toaster. Both of these devices are much smaller than those used by De Vries' patients. After a few months, the drives need to be serviced. When the warning light comes on, the service person disconnects the drive and reconnects it to another device as quickly as possible so that the user's heart does not sink. I watched the water in the tanks fluctuate rhythmically. It takes a lot of effort to push five or six liters of blood through the body every minute.
I asked how this heart sounds when it is installed in a person.
“Much quieter,” said Strain. “But you can hear him. I have heard stories in which patients say that when they open their mouths, other people hear clicks. " She told me that some patients at first could not tolerate the noise. But then, she said, "they couldn't sleep without clicking sounds."
We continued our way through the warehouse, where about a dozen hearts were stored on shelves, ready to be shipped. Surgical kits containing the materials required for their installation were packed in a separate stack. We then walked through the parking lot to another building, where a group of engineers were waiting for us wearing protective goggles in a laboratory with high ceilings. One of them handed me a small hourglass-shaped piece of plastic: spazz. Transparent, a little like milk, smooth, and sticky grippy on my fingertips. The spazz stretched almost surreal - I pulled on the ends, stretching the neck of the hourglass several times its original length, and the material returned to its original shape effortlessly.
Through the doorway, I saw a giant, worn-out car, about 3 meters high. She looked like an oil rig and a KitchenAid at the same time. "Spazz reactor," said Troy Villazon, production manager. "He's from the early 60s." SynCardia acquired the machine in the early 20th century to ensure a smooth supply of material. “This equipment has seen almost the entire history of spazz development,” Villazon said. We wondered for a while - was this very machine used to create Jarvik's hearts? “It's possible,” said Schuster.
I stopped in front of a blackboard on which four photographs of SynCardia patients were arranged above conventional hand-drawn diagrams. The photographs showed a black man in a hospital bed with a shopping bag; a balding white man on a golf course with a thin air hose coming out from under his shirt; blond, possibly adolescent, carrying a backpack; and young brother and sister sitting together. “We love seeing motivating pictures on the wall,” Villazon said. A nine-year-old boy was the youngest patient to receive a heart from SynCardia. The longest-lived SynCardia has been using the heart for nearly seven years - an achievement that could have been the cover of Life magazine in the 1980s.
One of the biggest challenges SynCardia faces is obsolescence. The Jarvik 7, on which the heart of SynCardia is based, was developed nearly forty years ago. The company's initial licenses are several decades old. Today, changing any single part - bolt, valve, resistor - may require new licenses. When suppliers go out of business or renew their offerings, SynCardia engineers must search, test, and then obtain authorizations to replace components. The company lives in fear of a fatal malfunction in the spas reactor: it could take a year to build and approve a new reactor, leaving potential new patients without hearts. Maintaining an outdated device is expensive. “Even if we do not improve or change it,we just need to keep producing the same stuff - people don't realize it, ”Schuster said. "I have worked in the aerospace industry and I can tell you that it is often easier to make major changes in aerospace projects than to change something in an artificial heart." I imagined how closely potential patients track the highs and lows of SynCardia.
There are fewer than twenty hospitals in the United States that have trained surgeons to perform heart placement. “This is a narrow market,” Don Webber, the company's CEO, told me. He took out his phone and opened a spreadsheet listing all the cardiac candidates at the time. “We receive lists every day,” he explained. “We get a phone call, text or email that says, 'We might have a patient.' On the phone screen, multicolored lines with patient data run.
SynCardia faces the same problem that Cooley faced in the sixties: you must be very sick to think about cutting your heart out of your chest, but if you wait too long and get sick, you cannot be saved. “There are cases like this,” Webber said with concern in his voice. “You see a person on the list this week, you see him on the list at the end of the week, you see him on the list next week. He just waits and waits and waits. " The longer a patient waits, the less likely they are to survive after an artificial heart implantation and any subsequent transplant. “This is not an easy decision,” said Webber. “There are several people on the team” - surgeons, cardiologists, hospitalists, and they all have to agree.
Business scientists use many different metaphors to describe invention and innovation. They say that technology can evolve continuously or discretely, that new products must climb the "adoption curve" or jump over the usability chasm. Nobody wanted to use mobile phones, but when they got smaller, everyone needed them. Electric cars seemed impractical, but hybrid engines gave drivers an opportunity to become familiar with technology and accelerated its diffusion.
Artificial hearts face unique challenges. Only those facing imminent death are ready to decide to transplant today's models. Yet nearly six hundred and sixty thousand Americans die of heart disease every year - a death toll at the level of a pandemic, although we are not talking about an emergency. An increasing number of people are living with heart disease and suffering from the consequences of these diseases. To reach their full potential, artificial hearts must be good enough for people to really want to use them. They should become preferable not to death, but to heart failure, as hip replacement is preferable to diseases of the hip joint. Until they reach wider distribution,they will remain a niche product - and therefore will not be available to the many people who need them. Another moment: Webber flipped through his list. I wondered if Jess should have been involved in this. Then he put the phone away.
SynCardia engineers have a responsibility to maintain legacy technology, but they also understand that it needs to evolve. Before I left Tucson, Villazon told me about the next generation heart that SynCardia was developing. This heart will use a new battery-powered pump motor that can be placed entirely inside the patient. Like the heart from AbioCor, it will be wireless, without an external drive. At the same time, it will pump blood using pre-existing spazz-based ventricles that have already been approved by the FDA. By connecting this new device to the old one (creating a hybrid model), SynCardia hopes to quickly develop and sell this heart to reach its existing customers. According to Villazon, the new heart can become a reliable and permanent implant.It can be used by people who are farther from the abyss.
I'm not Bud Fraser, but I've seen a lot of artificial hearts, and Villazon's device amazed me with its simplicity and originality. Yet SynCardia engineers have been busy manufacturing, selling, and renewing the current heart, saving over a hundred lives a year. They struggled to find time to start a new heart. They printed several 3D prototypes, sent specs to stores, and communicated with investors.
The Bivacor team from Cerritos is completely unconnected with the past of all these technologies. When I arrived, everyone was going to Tai for a weekly team lunch. It was a large group for a restaurant, but a small one for the design of an artificial heart. Timms sat at the end of the table next to electrical engineer Nicholas Greatrex.
“You are getting close to implanting your device in a person - how do you feel?” I asked. "Is it exciting, or weird, how does it feel?"
“The closer we get to transplanting a human heart, the more we think about everything that can go wrong and what we can do,” said Matthias Kleinheyer, a bearded engineer. "Even if I had no doubt that the system was working properly, it would still be very scary." Kleinheier is responsible for the backup systems. Heart has backups to backups to backups.
“Nick wants to live with the person who gets the first heart,” Timms said.
"Yeah," Greatrex said.
“If something goes wrong, we can fix it right away,” Timms said.
I introduced Timms, who was two decades younger and was tinkering in the garage with his father. Once the company sends its heart out for human transplantation, clinical trials, and eventually the market, its design must be carved in stone. The approval process was at odds with the improvement process.
“If I could, I would just keep working on this, this, and this,” Greatrex said. "I would never have implanted it." People were laughing, but he was definitely not joking.
If patients in need of an artificial heart can wait too long before deciding, the engineers who design them face a similar problem. If implanted too early, the device may not be perfect. If perfection is pursued, the device may not leave the laboratory. When we got back to the office, I spoke to Timms about wireless hearts. Investors have offered to give the company more money if it develops a wireless rechargeable heart right away. Gritting his teeth, Timms decided to drop funding, leaving wireless charging for version 2.0. “We would prefer to leave the money to make sure the device will work properly in the body,” he said. "If we test and tackle too many things at once, we will fail." He decided,that this was the most important design decision the team made. If removing the wires prevents the heart from spreading more widely, it could end all efforts. “I hate the drive connection so much,” Timms said. "I mean, this thing needs to be removed." But not right now.
In the lab, Greatrex introduced me to a technical innovation that the team was particularly proud of. The human circulatory system was inside the body, which was constantly changing its configuration in space. As a result of movement and application of forces to the body, the blood flow velocity changed. If you lie down, it goes down, if you get up, it goes up. Start running or jumping - your muscles will be filled with oxygen. All these movements pose a problem for the magnetic rotor at Bivacor. As the body moves and stops, and blood flow speeds up and slows down, the disc may be pressed against the walls. Ideally, the rotor should withstand the currents - float and rotate, as in zero gravity, keeping its position regardless of the circumstances.

On the board, Greatrex outlined the complex magnet control systems that the heart uses to sense and adapt to the forces around it. Timms himself developed the mathematical apparatus that made possible adjustments in solving complex hydrodynamic problems. The development process depended on digital technologies that were not available to previous generations of designers.
Greatrex gave me one of the rotors: it was a coin-shaped object, a few centimeters in diameter, made of polished gold-colored titanium. The team regrets that titanium will be a more practical gray in the final production version, he said. I weighed it. On one side in the center are eight metal prongs, similar to Stonehenge. On the other hand, eight curved, wind-blown triangles framed the edges, like sails or shark fins circling the world. An intricate swirl pattern filled the middle of the disc, machining marks like waves of the sea.
“I think if you showed it to a group of people, no one would understand that it is part of an artificial heart,” Greatrex said.
I turned on the light and took a photo. This object brought back some memories to memory - it was beautiful. It didn't look biological, but it didn't seem completely mechanical either. It had a kind of exquisite feature of something that had come a long way of development. In a sense, it was so.
- Russia's first serial control system for a dual-fuel engine with functional separation of controllers
- There are more lines of code in a modern car than ...
- Free Online Courses in Automotive, Aerospace, Robotics and Engineering (50+)
- McKinsey: rethinking electronics software and architecture in automotive

Vacancies
, , , - .
, , , .
, , . , , , , , .
, , .
, , , .
, , . , , , , , .
, , .
- -
- -
About ITELMA
-
automotive . 2500 , 650 .
, , . ( 30, ), -, -, - (DSP-) .
, . , , , . , automotive. , , .
, , . ( 30, ), -, -, - (DSP-) .
, . , , , . , automotive. , , .
List of useful publications on Habré