The peaceful atom, as we have already written, is not only Chernobyl and Fukushima . With competent and careful use, it can bring invaluable benefits to humanity, for example, when it comes to breakthrough technologies in the field of energy . But not only: today we will talk about radiation therapy for cancer treatment.
According to data from the Global Burden of Disease Cancer Collaboration study , which was published by an international team of scientists from 195 countries in the fall of 2019, from 2007 to 2017, the number of cases of cancer in the world increased by a third. In 2017, 24.5 million people fell ill with cancer, 9.6 million died from it. Radiation therapy has become the most dynamically developing method of cancer treatment. In terms of effectiveness, it does not lag behind other methods and at the same time is gentle on the patient's body.
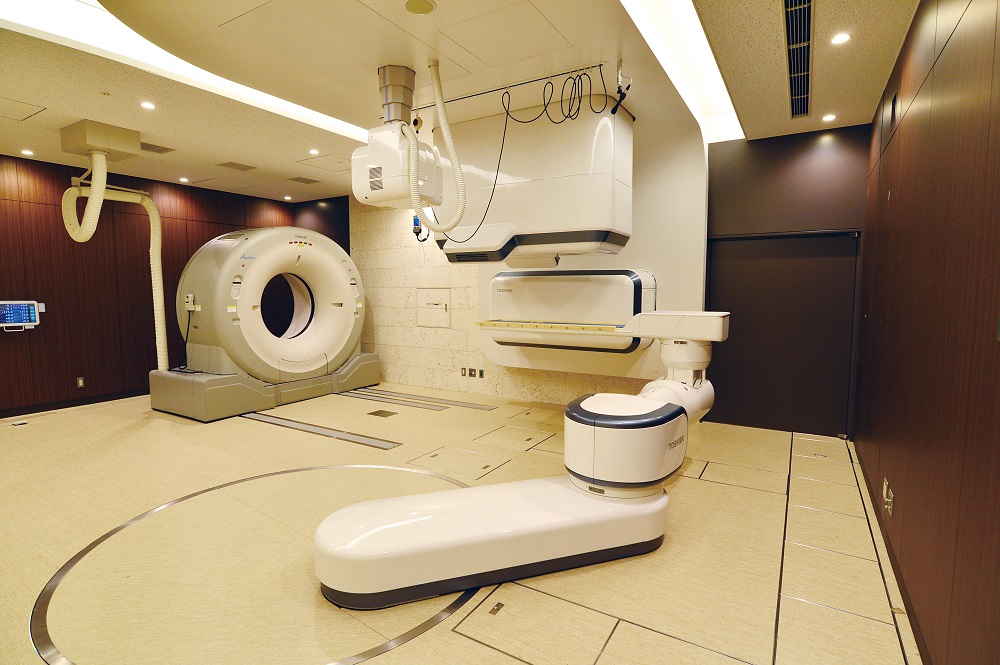
The room where the radiation therapy is performed (here - with the help of the i-ROCK apparatus) today may not look like a hospital room, but rather like a spaceship from the distant future. Source: Toshiba
How is cancer treated?
They prevent the division of tumor cells and its growth and spread of the disease throughout the body, as well as provoke its death. In general, a tumor can be removed by cutting it out of the affected organ or together with it, or poisoned by trying to make sure that the rest of the body is not poisoned at the same time. The latter, fortunately, can be done due to the nature of cancer cells. But chemotherapy, and even more so the removal of an organ or part of it, often affects the body very destructively. Therefore, scientists are working on alternative methods with scientifically proven effectiveness. One of them is just radiation therapy.
Radiation therapy (or radiotherapy) is the use of radiation to fight cancer. With the help of radiation, which is directed directly to the tissues affected by the tumor and affects its cells at the genetic level, they can be completely destroyed or at least restrain their growth and division. Despite the fact that these words themselves sound rather scary - to purposefully irradiate a living person with radiation! - this method has proven to be effective and safe.
The effect of radiation therapy is also based on the characteristics of tumor cells: as scientists have found, the fact that such a cell divides faster than ordinary cells leads to the fact that it is more influenced by radiation. On the one hand, fast fission allows them to spread at a high speed in the body, on the other hand, it makes it possible to introduce a kind of recognition system "friend or foe" and to influence radiation exclusively on them. As a result of radiation, the division of tumor cells slows down and / or stops, they disintegrate and are gradually eliminated from the body.
When a cell is exposed to radiation, the first task is to damage its DNA. As a result of this, the cell is inactivated, that is, it will lose the ability to divide, and as a result, this will lead to its death. In this case, the DNA molecule is completely destroyed in tumor cells and partially, without losing the ability to recover, in healthy cells. At the same time, modern technologies allow minimizing the effect of radiation on healthy cells. We will describe below how this is achieved.
Compared to surgery and chemotherapy, radiation therapy has several advantages. So, if chemotherapy affects the patient's body as a whole, which can significantly weaken it and give unpleasant negative consequences, then radiation therapy is aimed exclusively at the tumor and normally has only a minimal effect on neighboring healthy cells. Of course, in the case of a systemic cancer that has spread to multiple organs, chemotherapy may work more effectively.
If we compare radiation therapy with surgery, then here too the first one has an undoubted advantage: it does not require an operation, which in some cases will be difficult for the patient to endure, especially if his body is already significantly weakened by the disease and its subsequent treatment. In addition, it is not so easy to get to some tumors with a purely surgical method, and there is a risk of damage to neighboring organs.
Radiation therapy allows you to achieve the same result - complete disappearance of the tumor - without having to go under the knife. Best of all, this method of treatment works when getting rid of neoplasms that have not had time to spread throughout the body in individual organs, for example, in the brain, lung, stomach, prostate, and so on.
In modern oncology, radiation therapy can be used either alone or in combination with other methods of treatment - surgery and chemotherapy. In particular, a common treatment regimen is when surgery and radiation are used simultaneously.
In this case, there may be such types of radiation therapy: neoadjuvant (before surgery) and adjuvant (after surgery). Neoadjuvant radiation helps to shrink the tumor in order to bring it to a resectable state and reduce the risk of metastases, and adjuvant radiation is used to combat local tumor recurrence.
How does radiation enter the body and what harm can it do?
Irradiation of extremely harmful cells is a filigree work. The most important question that arises before a doctor can be formulated as follows: how can the particles be delivered to the right place and not accidentally irradiate anything unnecessary?
There are three methods of radiation therapy: remote, contact, and systemic.
Systemic radiation therapy means that radioactive drugs are injected into the patient's body (by swallowing or intravenously). They will be distributed through the bloodstream and act on tumor foci. So, for example, with the help of capsules that contain radioactive iodine, some types of thyroid cancer are treated.
When using contact radiation therapy (aka brachytherapy), radiation sources are placed either inside the damaged organ or in the cavity next to it. In some cases, the emitters can even be placed on the skin surface.
The most widespread method has become the remote method, when an external source of radiation is used, and healthy tissue can lie between it and the target. The latter receive minimal damage, since almost the entire radiation dose is released in the tumor at the last millimeters of the particle path. To achieve this, special devices were initially used, which, in simple terms, were a container with a radioactive substance and a mechanism that allowed the formation of a narrow beam of radiation.
One of the pioneers of this method of treatment was the Canadian medical physicist Harold Elford Johns - a group of scientists under his leadership in the early 1950s created the so-called "cobalt cannon", which used radioactive cobalt-60.
And the first special medical particle accelerator was assembled and used in London (Great Britain) in 1953. What for? To achieve greater penetration and efficiency of radiation and to reach deeply located tumors. And it is in the direction of the development of radiation therapy using linear particle accelerators that progress has been and is moving in the last half century.
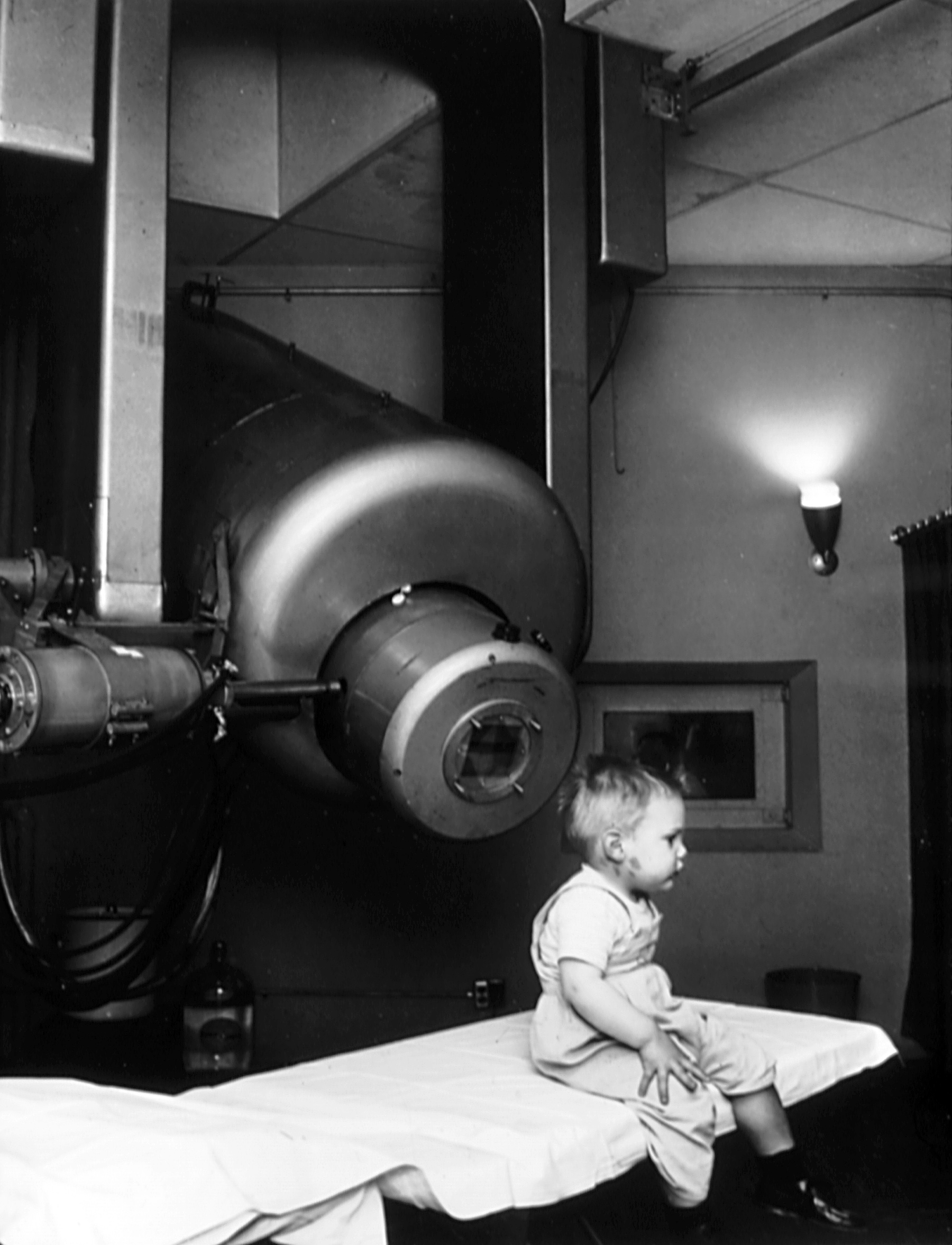
Gordon Isaacs, the first patient to recover in 1957 from retinoblastoma (a malignant tumor of the retina of the eye in children) using a linear accelerator built and used by the American scientist Henry Kaplan. As a result of the treatment, the boy's eyesight was saved, and he himself lived a long life. Source: Wikimedia Commons
Radiation therapy can be wave or corpuscular. Wave radiation, in which X-rays or gamma rays were directed at tumor cells, began to be used in medicine earlier (in particular, it was gamma radiation that was produced by the Jones cobalt gun), and in general it coped with its tasks, although it is impossible to direct radiation with wave irradiation clearly on damaged cells.
Today, corpuscular irradiation is considered more effective. In this case, beams of elementary particles are directed to the tumor: photons, neutrons or heavy ions. And it is irradiation with heavy ions that is currently considered the most technologically advanced method of radiotherapy, because due to their mass (it is not for nothing that they are called heavy) they form a kind of shock wave and therefore more effectively destroy the DNA of cancer cells - to successfully get rid of a tumor using heavy ions is required fewer radiation sessions.
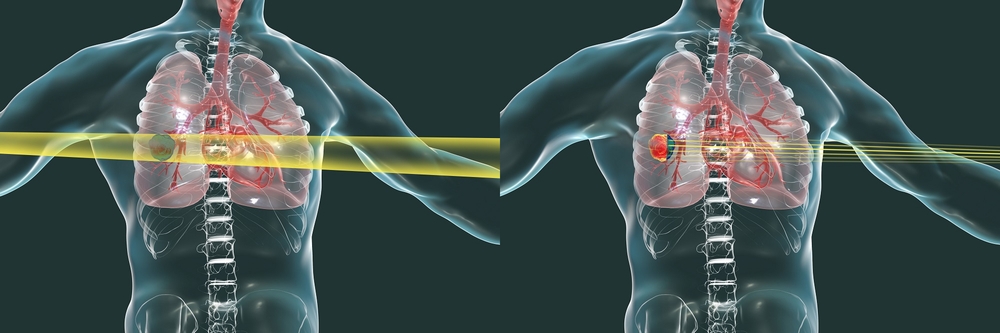
X-rays (left) and heavy ion beams (right). Heavy ions are directed clearly to the tumor, minimizing damage to healthy tissue. Source: Toshiba
As for other particles, they have less ability to penetrate into tissues. Therefore, the lightest of them - electrons - are used only for the treatment of skin diseases. The heavier ones - the photons - penetrate deeper, but still do not have the same impact force as the heavy ions. Photons are also used to treat tumors in internal organs, but with more radiation sessions.
Is radiation therapy harmless? Not. Despite the obvious advantages, like any intensive treatment, radiation therapy rarely goes completely without leaving a trace for the body. The consequences of its use can be local radiation burns, and the vessels that are in the immediate vicinity of the tumor can become more fragile. This leads to the risk of small focal hemorrhages.
Long-term side effects are also possible as a result of the release of tumor debris into the bloodstream. However, they are still not deadly - unlike malignant tumors. According to experts , the effect of the use of radiation therapy can be compared to a sunburn: its consequences are not always visible immediately, but may appear over time. Thus, there is a nonzero probability that after 10-20 years the patient may begin to change at the DNA level or the cancer will return.
What do the most modern radiation therapy units look like, or What can be done to treat more and better?
Three hospitals in Japan have already ordered heavy ion radiation therapy units from Toshiba, and the company has supplied the equipment to customers. And the heavy ion accelerator i-ROCK is successfully operating at the Kanagawa Cancer Center. On their example, you can see in what directions the evolution of methods of radiation therapy is going today.

This is how the actual heavy ion accelerator from Toshiba Energy Systems & Solutions looks like at the Center for Radiation Oncology in Kanagawa (i-ROCK). In the near future, a similar system will appear in Russia: a corresponding agreement has already been signed between the Ministry of Health of the Russian Federation and a Japanese corporation. Source: Toshiba
The i-ROCK is an impressive device that spans multiple rooms, the size of which is comparable to that of a gym. In it, with the help of a linear particle accelerator, a beam of heavy ions is accelerated to 70% of the speed of light before attacking a tumor. The amount of energy that is transferred to cancer cells significantly exceeds the amount of X-ray energy or proton energy.
Heavy ions come from two directions at once, which increases the effectiveness of treatment, that is, it allows you to kill the tumor in fewer sessions. Moreover, the emitters can be rotated 360 degrees, due to which a high accuracy of exposure is achieved.
Modern installations, including i-ROCK, have learned to minimize damage to healthy tissues during irradiation. To do this, it was necessary to make the particle beam thin and the radiation power sufficient to damage the tumor, but not the tissues around. I-ROCK uses a method of 3D scanning of the tumor, thanks to which it is possible to attack only the tumor itself, no matter how complex its shape, with high accuracy. This is called High Speed Scanning Beam Irradiation.
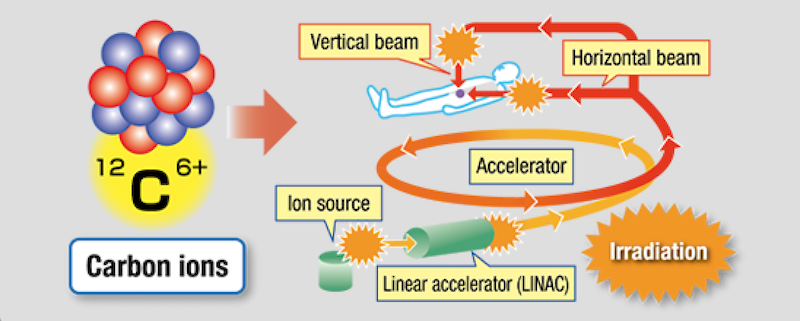
We take carbon ions, strongly accelerate them in a linear accelerator and direct them into the patient's body, but not somewhere, but exactly at the target. Source: Toshiba
Using Toshiba's 3D scanning method during heavy ion therapy, the tumor is irradiated as if it were shaded with a thin pencil. This method allows you to act on tumors of complex shapes and act with high precision and efficiency. Another consequence of the application of this method is that it is possible to exclude the stage of long-term equipment adjustment and the use of collimators and filters, which must be made individually for each patient.
But what to do with organs that normally move, as long as their owner is alive - for example, with the lungs? On inhalation, the tumor in the lung will be in one position, while on exhalation, healthy tissues will appear in its place under the beam. To avoid this, Toshiba engineers have added a tool to monitor the patient's body in real time to the installation, allowing radiation to be turned on when the organ is in focus of the emitter, and turned off when it moves. By combining breath-synchronized irradiation and real-time oblique radiograph observation with re-scanning technology, Toshiba engineers have learned how to quickly and accurately irradiate neoplasms with uniform doses not only on motionless, but also on moving organs.
. : Toshiba
Among other things, such a combination of technologies and methods, on the one hand, makes it possible to reduce the preparation time for treatment and its cost for the patient, and on the other hand, to increase the number of patients that the hospital can admit during the reporting period, and, consequently, to accelerate the return on investment. Toshiba has helped reduce the time it takes to position the patient by creating an efficient positioning system, and the overall time spent in the therapy room is significantly reduced with the use of high-speed 3D scanning radiation. The Toshiba Positioning System automatically calculates the discrepancy between the CT scan of the irradiated area obtained during treatment planning and the X-ray taken directly in the room where the irradiation is taking place and adjusts the position of the robotic bed.on which the patient is located. Whereas when using the previous generation of radiation therapy devices, the average session duration from the patient's entrance to the room to his exit was 26 minutes, now it has been reduced to 11 minutes.
Finally, another area of work for engineers is to reduce the weight and size of the entire set of equipment, which in turn ultimately again increases the availability of treatment for each patient. Here, Toshiba also has something to be proud of: it has created the world's most compact (as of October 1, 2017) rotating gantry (the so-called mobile device used to hold and aim medical equipment at a fixed patient), used in heavy ion therapy. This was achieved through the use of superconducting technologies. If the gantry can rotate 360 degrees around the patient, this allows you to accurately aim at the tumor from any direction, reduce or eliminate damage to healthy tissues, quickly position the patient in the right way and reduce his discomfort.and at the same time, to exclude organ deformation as much as possible; moreover, subsequently, during the next irradiation sessions, the patient's position can be quickly reproduced.
Scientists from the National Institutes for Quantum and Radiological Science and Technology (QST; a Japanese research organization created in 2016 through the merger of the National Institute for Radiological Research and several divisions of the Japan Atomic Energy Agency), in June 2019 created a compact rotary gantry using a superconducting magnet, which reduced the weight of the equipment by about 300 tons. The smaller and lighter gantry can be more conveniently placed in the hospital building, and this will reduce the costs of construction, maintenance and service, and therefore, will reduce the cost of treatment.
Finally, it is worth talking about how the safety of treatment is ensured. First, the accelerator and the patient are in different rooms. The latter is located in a separate, not at all scary-looking room (shown at the beginning of the post) on a bed that can be moved along seven axes to provide irradiation of any organ and at the same time maintain a comfortable position for the patient. The optimal position of the bed and emitters, as we have already mentioned, is determined on the basis of a preliminary computed tomogram and real-time X-ray scanning just before the start of the procedure.
The healthcare professional can monitor the treatment using the Toshiba Beam Monitoring System: while the irradiation continues, the position of the beam and the flux density at each area of the irradiated tissue are displayed on the monitor screen in the control room in real time. The condition of the equipment is also constantly checked to ensure the safety of the patient. If something goes wrong, a special blocking system will stop the flow of particles. The equipment control interface has been specially designed to minimize the possibility of human error and give healthcare professionals a sense of confidence and safety.
Is radiation therapy ruinous?
Like any new technology, in the development of which a lot of funds and efforts of highly qualified specialists have been invested, radiation therapy cannot be cheap. For the patient, the course of treatment will cost on average more than the course of chemotherapy (exact calculations depend on the severity of each case).
The high cost is understandable: first, hospitals need to invest in expensive equipment. Secondly, its maintenance will require additional costs. Thirdly, to work on it, you need personnel with a high level of qualifications - you will also have to spend money on its training and maintenance.
As for the cost of the equipment itself, the scope is very wide. So, the simplest, not the newest, and, possibly, a used linear accelerator abroad can cost up to $ 300 thousand. Newer systems go up to a million dollars and more. Moreover, the latest developments can already be estimated at several million US dollars. In general, for a full-fledged equipment for a radiotherapy clinic in the United States, for example, you will have to spend from $ 20 million to $ 150 million, and in some cases even more. It depends on the number of seats and other factors.
Nevertheless, any effective technology over time goes the same way: it becomes mass, and as a result - more accessible. And we hope that the “terrible and dangerous” atom will clear its image in the near future and turn into the savior of humanity from one of its most terrible problems.