Someone left me a piece of an instrument in the root canal.
Perhaps, as a child, you thought that doctors are kind people who are guaranteed to cure you. The adult world should have already convinced you that there are not enough competent people in any field. In the case of dentistry, fortunately, it is quite difficult to kill a patient unknowingly. But on the other hand, it is easy to harm health, which is then very expensive and long to compensate.
The problems are absolutely the same as in critical areas of medicine: underdiagnosis, overestimation of one's own manual skills, incorrect recognition of a clinical case (as a result, the wrong choice of treatment method), just crooked hands, non-compliance with standards and a malicious increase in the bill due to the desire to earn, contrary to the interests of the patient.
Let's start with underdiagnosis and overdiagnosis. “Inadequate” - this is when you came up with a problem, the doctor closed only it, but did not say that there are a few more things that need to be done now, so as not to lose teeth later and not to install expensive implants. The phenomenon is very typical for dentistry: you did not ask, the doctor did not say. Try this with a cardiologist. "Over-" is when, based on the results of the examination and the first instrumental methods, an excessive number of examinations are assigned. To some extent, this is even good for caring for the patient, but only as long as we are not talking about excessive radiation exposure or the desire to sell more research when it is not needed according to the indications. Or overtreatment: expanding the indications for treatment, for example, how you could have given pills, and your ears were cut off, because it was more expensive.
As a result of the diagnosis, a treatment plan is born. In case of expensive interventions, the patient does not trust the doctor, so he goes to another clinic. A day later, the situation "three doctors and six treatment plans" is formed, which confuses even more.
Why is there underdiagnosis?
Because there are no protocols in commercial medicine in Russia. More precisely, they seem to exist sometimes, but in fact they are still not there. In the case of critical diseases in the CHI there is a scheme of indications that unambiguously lead to certain analyzes and studies. If the patient noted something in the history, it was entered on the card, and a study was not prescribed for such a case, then the doctor may even go to jail after the trial (this happens rarely, more often it is about serious fines to the clinic from insurance funds).
That is, for every critical case that threatens life or health, there is a diagram. This is important for the state, because the cost of a citizen's life, in fact, can be considered as underproduced GDP, that is, as unfinished work during this expected life. Quality of life is usually viewed not as compulsory medical insurance, but as voluntary medical insurance or commerce. In the case of quality of life, there is no such scheme. Dentistry is extremely rare about a threat to life: perhaps these are rare oncologies and various interesting infections from the teeth to the brain. In all other cases, you can throw the tooth into a basin and give an anesthetic. 15 minutes, 220 rubles - that's roughly how much it costs for an OMC clinic.
Small regional clinics, where patients come to complain of a toothache or a piece of tooth that has fallen off, are rarely engaged in the diagnosis of the same root canals. For me, who is well acquainted with European medicine, it is simply wild that a doctor might ask:
- Well, patient, what will we treat?
In a normal scheme, the doctor makes a diagnosis and himself says what he is planning to do now. The patient can agree or refuse, sometimes - choose an option.
On the one hand, it is beneficial to do a complete diagnosis: it increases the check, because you can persuade the patient to at the same time cure caries at an early stage, which he did not know about. On the other hand, the patients themselves do not like this, because they believe that this is a way to "breed" them for additional money. And they are not always wrong. Another feature is when the clinic's marketer gives the task to load the CT machine, because it slowly pays off. At this point, the number of additional studies on it begins to grow.
In my clinic, there are only protocols and case selection. That is, any patient always undergoes the same diagnosis. If a pathology is determined, the next "case" with additional methods for it is immediately selected. No creativity, no gag, in two identical cases there will be absolutely identical research sets. This diagnostics is somewhat redundant in comparison with OMC standards, but we are working in an expensive segment: our task is not to heroically solve problems, but to remove them before they appear. Patients understand this very well (in our case, such a reputation appeared about two years after the start of work).
The simplest example of underdiagnosis is not to take interproximal images, that is, not to see caries.
Hasn't proven the importance of treatment
The next mistake is that the patient's tooth root is rotting, but he does not want to heal. More precisely, this is not entirely a mistake, but rather a consequence of the entire medical system in its current form. People do not trust doctors because they suspect them of incompetence and greed.
The doctor rarely says exactly what is happening. Very rarely explains what he does and why. And almost never can justify the treatment plan in terms that the patient understands. European dentists in this regard may be similar to ours, but there the degree of trust in a person in a white coat is so great that they may not particularly dive into details. Oddly enough, in our small clinics, the owners often behave like psychotherapists, literally carry the patient in their arms, but only the owners, not the line staff.
We decided for ourselves that we would keep the patient informed of everything that was happening in great detail. Since we are working with an expensive segment, people appreciate this sense of control over the project. And confidently make decisions based on all the data. It takes a lot of extra time, but we do not have a quota, as in the OMS.
If the doctor was unconvincing, then the patient postpones treatment or goes to the next one for advice. If it suddenly coincides that there will be underdiagnosis, then the situation is quite possible: “What are the roots? You have two caries, you can see them with your eyes. You are being bred there, let's drill now, and everything will be ready in half an hour! " Unfortunately, I cannot deny that they are really bred somewhere.
Example: often women notice that their mouth is literally all collapsed after childbirth. There is often a fairly simple story. By the age of childbearing, the patient comes with her teeth in a borderline state: for example, until the age of 30 she was in dentistry five times, and the last three times she did not take pictures. Then she stays at home for two years and does not go to the dentist at all. As a result, in two years the doctor will not convince her that it was not because of pregnancy, but simply because it was necessary to think about health sometime earlier. This is the problem of at least the doctor who had her last before pregnancy: he had to make a diagnosis and convince her to be treated.
In Russia, a decision on a patient is often made by a doctor who spoke more convincingly. And he sometimes talks with a blue eye. As a result, many excellent medical professionals who are unable to speak to the patient often suffer commercially.
Wrong choice of "case"
Evidence-based medicine, based on mathematics and scientific approach, involves the following:
- The patient is sufficiently fully diagnosed to make a decision.
- Diagnostics is performed until a specific case (diagnosis) with clarifications is determined.
- For this case, there is a choice of several treatment options: you need to evaluate each in accordance with the characteristics of the patient and the nature of the case, the capabilities of the doctor and clinic.
- After choosing an option, you need to implement it as efficiently as possible.
That is, with the correct diagnosis, the choice of the doctor's actions is based on a statistical assessment: "If this method in such a specific case shows the result of success higher and less risks, then we take it."
The problem is that the method is evaluated not only as a type of intervention, but also as an opportunity to implement it. Some operations require very good manual skills of the doctor. Some methods require expensive equipment and materials, and replacing them immediately changes the likelihood of success. Some methods are expensive for the patient, and he will not be able to choose them. Some cases are highly dependent on the patient's health condition, for example, previous diseases and age.
Only very rarely at the forefront, patients come with "Doctor, what have I got?", And the doctor says:
- Oh! What do you have?
We have this more often than usual, because we are doing scientific research. My colleague Huseyn, for example, accepts children with narrow upper jaws from all over the CIS (and treats similar cases in Italy). There is a place for creativity and experiment, but with the consent of the patient.
If a doctor treats teeth in Africa, then, probably, the case selection boiled down to "pull out like this" or "pull out with partial anesthesia with alcohol."
To summarize, in the phase between diagnosis and intervention, it is important not to overestimate your capabilities and skills. The problem is acute for us, because we often retreat what the doctors taking courses on YouTube have done. In surgery, knowledge should not be confused with information. You need to do the operation several dozen times with the assistance of an experienced colleague and only then take it yourself.
I also often see an overestimation of the severity of the condition. Here - the question of money: aggressive marketing of manufacturers of implants often moves training in the direction of "tooth to hell, we put the implant, it is all that matters." Again, for my clinic, I chose the paradigm of maximum tissue preservation during treatment, that is, we save teeth even in very difficult situations. The paradox is that in our performance it is often more expensive than pulling out a tooth and placing an implant in a regional clinic. Usually in the clinic it is a little more expensive, but less marginal than implantation.
And a very interesting case is when one doctor chooses a treatment plan at the border of specialties. If in the clinic the therapist is stronger than the surgeon, then there will be many preservation of teeth. If the surgeon is stronger than the therapist, there will be many implantations. There are no consultations in dentistry, so just remember that the first doctor will determine what will happen to you. And surgeons tend to cut something off.
Yes, there is also a downward choice, when an intervention with a minimum of risks is chosen for a difficult situation. For example, in the compulsory medical insurance, they strongly scold for getting a patient from the clinic to the hospital. That is, the doctor's task is often reduced to ensuring that the patient does not end up in the hospital at any cost.
Crooked hands
The next mistake is simple and straightforward: the surgeon was wrong.
The situation here is twofold. On the one hand, Russia has traditionally strong surgery. On the other hand, Russia is a country of home-grown dentistry. They teach us from textbooks of the 60s of the last century. As a doctor graduated from the university, he sits there, and heals using the same methods as taught. If you need to go through something new, he either tries it himself or pays for expensive refresher courses. The latter happens less frequently in the regions, and almost never happens in compulsory medical insurance. As a result, objectively, you can quickly learn either from homeless people (I'm serious: we are talking about charitable treatment of the most severe neglected cases with information about its nature), or from unsuspecting paid patients.
Since often the powerful surgery of the 60s is combined with a lack of money, we see completely wild things that patients bring in the jaws. A paperclip instead of a titanium pin - please. The pin is expensive, and the paper clip is pretty much the same, isn't it? Or here's a wedge - it's actually for someone else, but our doctors have ways to take any device and use it for other purposes. The main thing is that it has similar physical and chemical properties. This causes both admiration for ingenuity, and disappointment, because sometimes it gives side effects, but we can heal.
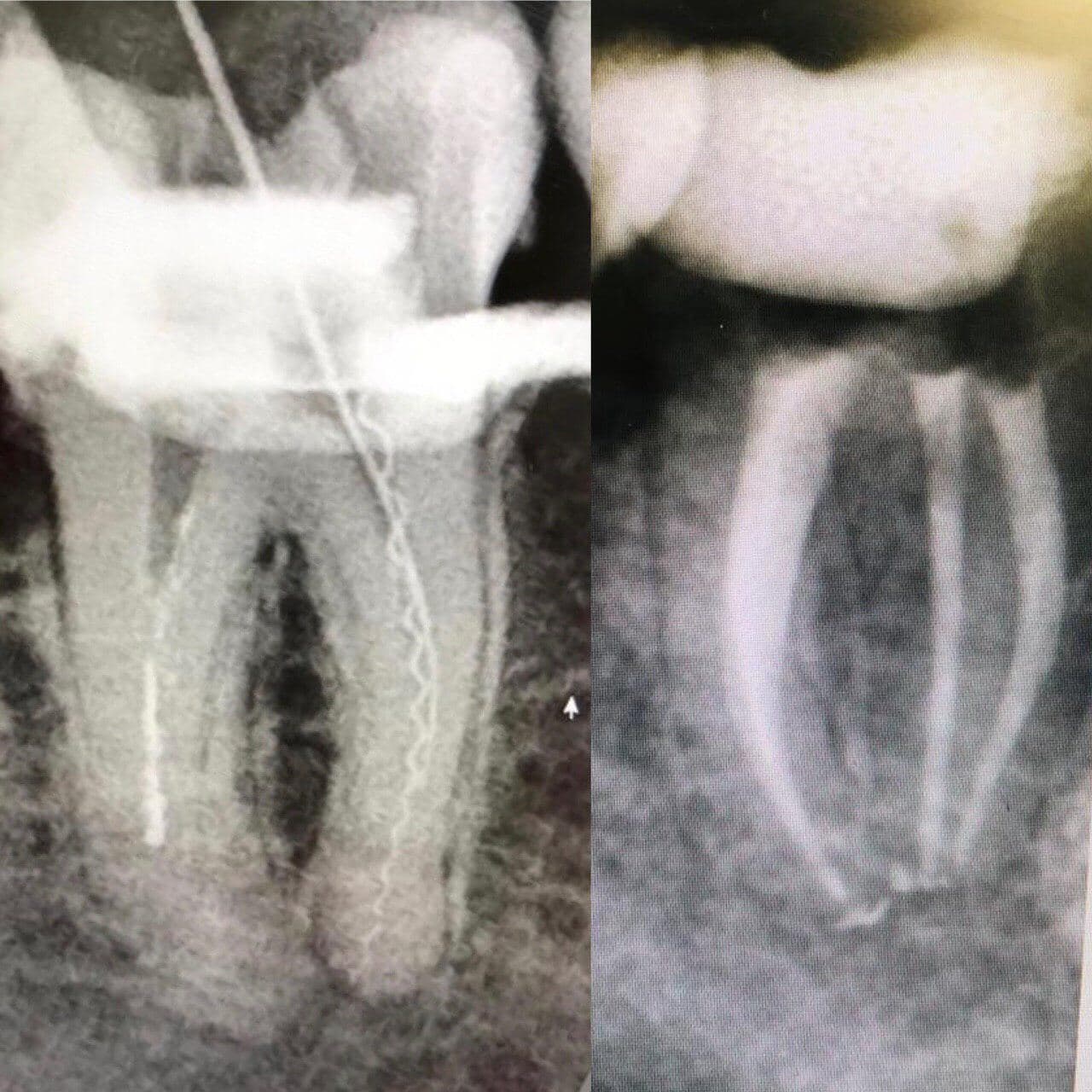
Doctors often break an instrument in the root canal. You rarely know about this. The fragment is often "buried" directly under the filling material. Then it all depends on what kind of tool it is: it was infected or not, it was bypassed further during the intervention or not. The most common find I find is a broken canal filler. This is such a spring, it is driven to the top of the root, then the motor is turned on, which cannot be done in such a situation. It breaks down. Leaving it in the channel is not entirely safe, but it is often safer than taking it out.
Sometimes patients come from business trips with traces of complete economic despair. If in the north of the country in a small settlement with the prospect of oil and gas production there is only a paramedic center, then they will treat as best they can. My patient brought a hefty sewing needle: the doctor told him that he has inflammation, and he needs to poke the needle with a swing into the tubercle to get the pus out. It sounds barbaric, but the decision in his situation is correct: due to the lack of tools or skills, he provided an effective way to prevent the death of a patient due to complications of infection. And I've already cleaned everything up in Moscow.
Failure to comply with protocols (let me remind you that there are no official ones) can also be attributed to crooked hands. At this point I want to go back to the rubber dam again. If you do not isolate the tooth, then saliva, air from the respiratory tract and a lot of all debris will get into it. This is not only necessary, but a natural and necessary step in many interventions. For example, in the case of veneers, an isolated tooth is much more likely to remain in contact.
And this is just one example of a protocol. We often have things like “treat with drug # 1, inflate and expose it for 10 seconds, then with drug # 2 in such an amount, but do not inflate and leave on top for 20 seconds, then inflate the third and inflate, then place the structure in the solution, dry and glue. " Skipping an item or performing it incorrectly leads to the fact that something is peeling off.
When implanting, it is important not to drill too quickly: this can cause overheating of the bone, and after two weeks necrotic changes will begin there. That is, there will be a dead bone around the screw, which will sadly affect the success of the operation. The "coffin of dead cells" is a fairly classic cause of problems with old implants.
Since doctors do not use math or statistics, most error cases fall on technology. But the matter is simple: if you know that the method, when used correctly, gives 98% success, 3% side effects and 0.2% irreversible side effects, and you had 18 patients with this in the clinic in a year and only 12, and two more - with serious side effects, then, perhaps, it is not the method. Perhaps the fact is that this performer is afflicted with a rare genetic disease simlicitum. "The implants did not take root" - this is it. Even a rusty nail takes root if protocol is followed.
But, since there are no one hundred percent methods (we joke that even a hairdresser's haircut has a chance of success somewhere around 92%), and statistics and a very accurate choice of case still need to be confused, a lot is done by eye. This is neither good nor bad, it is a matter of approach. My approach is to rely on data as much as possible when making a decision and verify the results afterwards.
Partly the case of crooked hands can be attributed to the lack of the necessary equipment. I wrote about microscopes and their obligatory use in the clinic last time... For this we are still not liked, because the microscope requires retraining and reveals the smallest errors. Plus, video recording reduces self-esteem during parsing. But it provides tremendous benefits, including numerical success in treating inflammation. By the way, from a number of clinics I know that the presence of a microscope and an intraoral scanner does not guarantee that a doctor will work with them: it is far from a fact that he will not be more accustomed to it, as in the 80s.
In Russia, it regularly comes as a surprise to me that the clinic does not have an autoclave. Tool sterilization is just a basic thing. Moreover, it is needed for licensing. That is, they brought the autoclave, showed it to the inspectors, and took it back to some other clinic. The advice is simple: if you happen to have to treat your teeth in a small clinic, then ask directly how the instrument is sterilized. For this, the packages have labels. It works like this: after pre-sterilization cleaning (disinfection), dirty instruments are put into bags for an autoclave, then they are heated in it, and the mark on the bag changes color at a temperature peak. You need to make sure that the tool is taken from the bag with the green label with the letter S showing through. There are other variations of the labels, but this is the most common.Good assistants do this with the juicy sound of opening the bag right in front of the patient's face.
This is what the label looks like before sterilization, it is reddish-brown:

And this is how it looks after sterilization, green, you can see the letter S:


But here I must say that autoclaving is necessary for common infections, we are not necessarily talking about hepatitis or HIV. Their pathogen is unstable, and in fact, it is quite possible that it will simply fall apart between the intervention of the same instrument in two different patients. I do not urge you to work with a dirty tool, and now I will explain why such clinics do not close immediately after the first sick person: because if the disinfection protocol is not followed, the sick person may not last long. This is not a canteen where there are a dozen cases of poisoning at once in one day. There is no blood transfusion in conventional dentistry.
And further. If your braces have not been removed for two years, it was an orthodontist's mistake, and now they are trying to fix it. I had a patient who, at the time of the first appointment, had been wearing braces for six and a half years: it seems to have been three mistakes on him. They helped, of course, for another year and a half, but it was difficult for a year and a half. A total of eight years of braces.
Malicious increase in score
The first case is simple: a star surgeon from Moscow comes to a small city, and he needs to fill 108 patients. There are 105, three more would not hurt, and now someone who could save a tooth goes to implantation.
The second case is more interesting, one of my specialists had this (and he is still terribly ashamed of this part of the work in the previous clinic). The doctor received a percentage of the materials sold. The most valuable is gold. Pins are made of gold to strengthen the tooth before installing the crown. You can not do strengthening, but work very carefully under a microscope. A thin gold-palladium alloy pin can be fitted. Or you can pick up more tissue and put a larger pin.
The larger the pin, the higher the doctor's salary. It turns out that he is interested in removing as many fabrics as possible in order to put a heavy tab. The clinic benefits from this, and she believed that all teeth with a crown should be restored with a pin insert. In my opinion, this is a serious managerial mistake: it can increase profits for a year or two, but further the reputation of both the clinic and the doctors will be bad.
If the clinic has a free consultation for retirees, there will often be something aggressive, often misleading. Is it worth a 40% discount on services and designs? This is a deception - well, or the doctor is just learning. The only normal case that I have seen is when they directly write that the doctor is new, he needs to be downloaded, and therefore on Thursdays - free consultations.
There are methods with unproven effectiveness or insufficiently researched. There are limited-use methods that can be scaled up with a multiple increase in the risk of side effects. This is often seen on implants: "Now we will pull everything up - I will put the implants, everything in a week." The method is called all-on-4, all-on-6. It is very good for a number of rather narrow situations, but now it will be spoiled by would-be doctors who use it everywhere. Because it's cheap and fast, patients are very easy to convince. Do not be afraid of the doctor, all at once, the teeth are white, beautiful. And the insidiousness is that the work can be finished with a temporary structure made of plastic: it is needed as a way to chew while the permanent structure is being prepared. The first year it looks very beautiful, but its biocompatibility is not very good. Then wear begins, bacteria settle in the cracks, and the smell begins.And then it all starts to fall apart. Several decades ago, there were still nylon prostheses, also the same story. But I haven't seen them for a long time.
Why is that? Do the doctors want to deceive you? Everything is bad?
I know that in this place it is customary to scold the country and the medical system.
No. The medical system is generally in order. You can work. There are problems, but other medical systems, with all their advantages (as in the USA with protocols), can have other fatal disadvantages (as in the USA with policies).
Our problem is that we don't trust teachers. They learned old things without access to technology. The past generation of doctors cannot teach because they like to work without a modern scientific approach. The new generation lacks experience, skills and deep knowledge. The result is a gap, which we are now smoothly closing.
In the 90s, businessmen sat down on the ears of doctors. This changed the way of selling and caused overdiagnosis and retreatment. We knew one company that made a great medical system. At some point, a large holding bought them, kicked out doctors and launched marketers. They expanded their indications and started selling aggressively. The result is that the system has discredited itself. The patient does not need a system, but a doctor who will make an objective decision.
Prophylaxis is poorly developed; in the country as a whole, we like to treat according to symptoms. This can and should be corrected by informing and just examples of work on diagnostics.
Science is driven only by enthusiasts, there is no framework for collaborative research and testing, as in Europe. This is perhaps the most important strategic part, but my doctors conduct research outside the Russian Federation, publish and teach, too, more often not in Russia. This is what will potentially slow down medicine the most: if a doctor is not paid for new technologies and research, then he goes to earn money himself or work outside the country. And now only commercial medicine and only the cutting edge can pay.
Thanks for attention! Now you know a little more about how dentists treat you. And you can roughly shift this to other areas of medicine.