Herd immunity varies from one locality to another, and many factors affect its calculations
It is difficult to calculate the time when the disease ends spread in the population
While many aspects of the current pandemic coronavirus remain unknown, one thing we know - it will end, when the spread of the virus will start to slow down, and eventually almost stopped due to the fact that enough people will develop a him immunity. Whether this happens because of the emergence of a vaccine or because of the spread of the disease - as a result, the population will have " herd immunity "
“As soon as the level of immunity exceeds a certain threshold, the epidemic will decline, because it will not be able to find enough new people to become infected,” said Natalie Dean of the University of Florida.
Determining this threshold for coronavirus is extremely important - however, there are many nuances in calculating the exact percentage of people who must acquire immunity for herd immunity to appear, which protects people who have not yet been ill.
At first glance, everything is simple. The only thing you need to know is how many people an infected person infects on average. This value is called R 0 . After that, it only needs to be substituted into a simple formula for calculating the herd immunity threshold: 1 - 1 / R 0 .
For example, for a coronavirus, the R 0 value is 2.5, that is, on average, each patient infects two and a half people (this is a common estimate). In this case, the threshold for the coronavirus is 0.6, or 60%. That is, the spread of the virus will accelerate until 60% of the population acquires immunity.
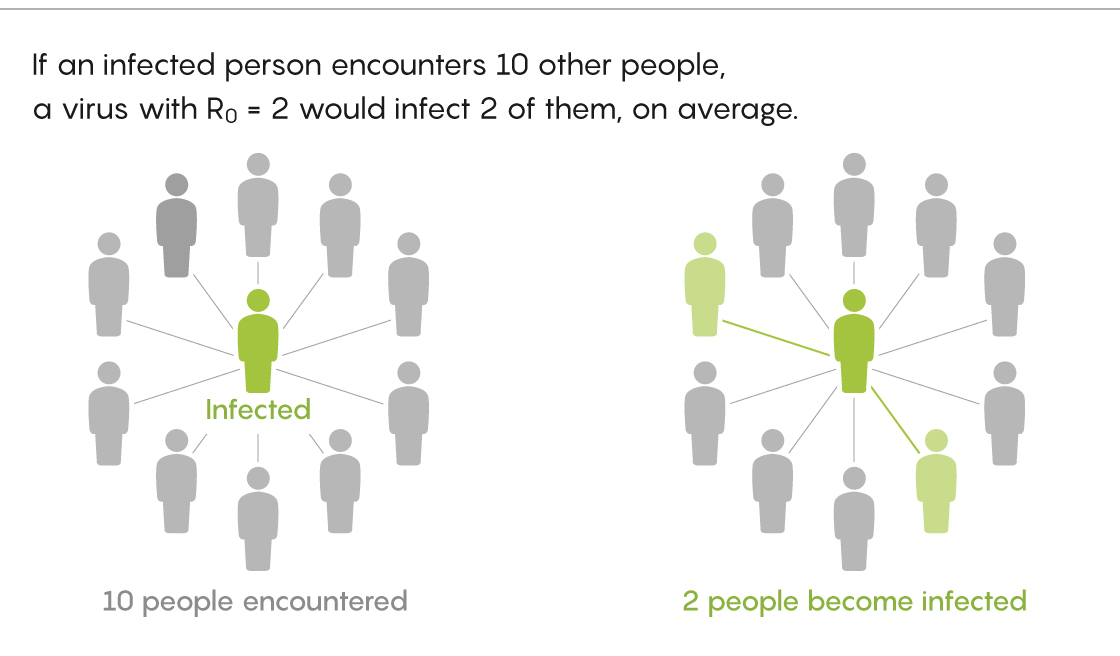
If R 0 = 2
After that, the virus will continue to spread, but at a decreasing rate, and then will stop spreading altogether. Just as the car does not stop immediately after you take your foot off the gas pedal, so the virus does not disappear after herd immunity is achieved.
“You can imagine that after 60% of the population is infected, the number of infections will begin to fall. However, until the disease begins to disappear, another 20% may become infected, ”said Joel Miller of La Trobe University in Australia.
This 60% also denotes the threshold after which the new appearance of infection - when, say, a sick passenger leaves the ship and ends up in a healthy port, where there is already herd immunity - will quickly disappear.
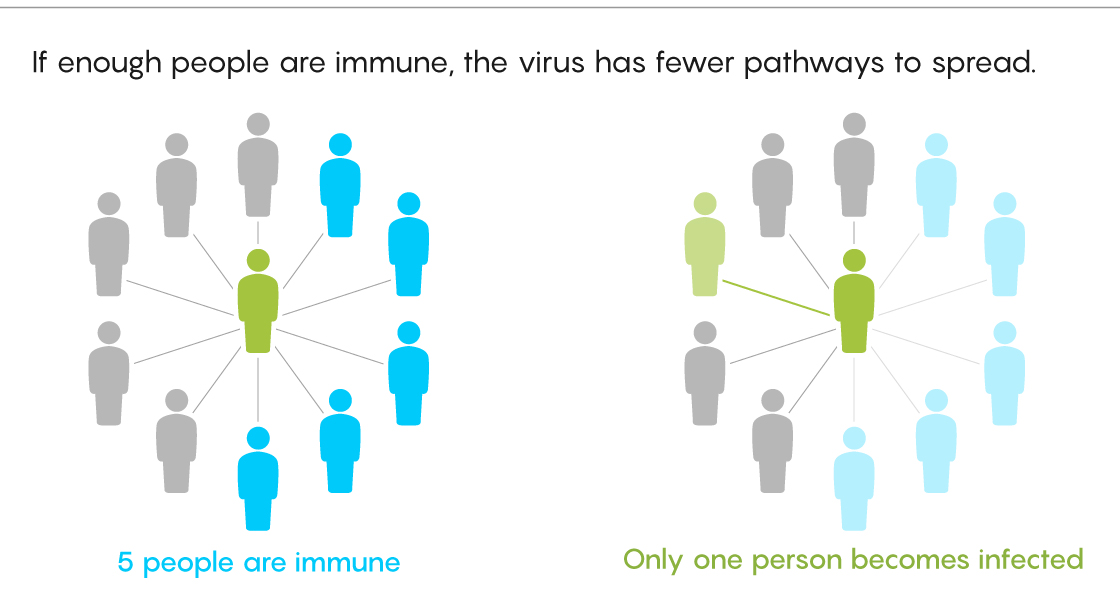
If enough people have immunity, the virus will have nowhere to spread.
“This does not mean you cannot light a fire, but this outbreak will simply fade quickly,” said Keith Langwig of Virginia Polytechnic Institute and State University.
However, things get more complicated further. The herd immunity threshold depends on how many people one patient actually infects - and this number may differ from one locality to another. The average patient living in an apartment building will infect many more people than the average patient in rural areas. So if R 0for the coronavirus, the world average will be 2.5, on smaller scales it will vary significantly. This means that in some places the herd immunity threshold will be much higher than 60%, and in some it will be lower.
“I think the range of R 0 values for coronavirus is much wider than people think,” said Mark Lipsich of Harvard University, who advises health officials in Massachusetts and abroad. According to him, in some cities it can be twice as high as the US average.
Just as R 0 turns out to be a variable rather than a constant coefficient, so the method of acquiring immunity by different people varies - and this greatly affects the calculation of the threshold of their herd immunity.
Researchers usually talk about herd immunity in the context of vaccination. Many of these campaigns assume that everyone has the same chance of contracting and spreading the disease. However, with the natural spread of infection, this is not always the case. Differences in social behavior make some people more susceptible to infection than others. Biological differences also play a role in the likelihood of infection.
“We are all born different, and then, as we accumulate different experiences throughout life, these differences accumulate,” said Gabriela Gomez of the University of Strathclyde in Scotland. "It affects how well each person can fight the virus."

Gabriela Gomez of the University of Strathclyde in Scotland
Epidemiologists refer to these variations as "susceptibility heterogeneity," referring to the differences that make people more or less likely to contract the disease.
However, for vaccination campaigns, these are too complex subtleties. “Distribution of a vaccine to a population usually doesn't take into account how many contacts or how susceptible they are - we just don't know that,” said Virginia Pitzer of the Yale School of Public Health. Instead, officials prefer maximalism, and, in fact, vaccinate everyone.
However, since there is no guarantee that a new vaccine will appear in the near future in the current pandemic, the heterogeneity of susceptibility seriously affects the herd immunity threshold.
Sometimes it raises this threshold. This is possible in nursing homes, where the average resident is more susceptible to coronavirus than the average resident of the country.
But on a larger scale, uniformity tends to lower the herd immunity threshold. At first, the virus infects more susceptible people and spreads faster. But in order to continue to do this, he needs to move to people who are less susceptible to him. As a result, it is becoming more difficult for the virus to spread, and the epidemic is growing more slowly than one would expect based on its initial growth rate.
“The first person is likely to infect the most susceptible people to the virus, and the less susceptible people will remain in the second half of the epidemic - in the end, the infection will be coped with faster than you think,” Lipsic said.
Evaluating uniformity
So how much lower is the herd immunity threshold if the virus is spreading everywhere, as in the current pandemic?
According to standard models, about 60% of the US population will need to get vaccinated against coronavirus or get sick with it in order to slow down and eventually stop the spread of the disease. However, many experts I interviewed suspect that the threshold for naturally acquired immunity is actually lower.
“I think it will be somewhere between 40 and 50%,” Piczer said.
Lipsic agrees: "If I were asked to make a guess, I would stop at 50%."
All this is just guesswork from the data, since it is very difficult to quantify what exactly makes one person more prone to disease and another less. Many of the characteristics you might think of - the degree of social distancing, for example - can change from week to week.
“This whole homogeneity task only works if the person has long-term sources of that homogeneity,” Lipsic said.
Uniformity can be difficult to assess, however, it is one of the important factors in determining the herd immunity threshold. Langwig believes that the epidemiological community has not done enough to make an accurate estimate.
“We are a little lax about herd immunity,” she said. "This variability is important, and we need to be more careful in assessing the herd immunity threshold."
Several recent works have attempted to do this. In June, the journal Science published a study using a fairly modest percentage of homogeneity, and estimating the CM threshold for coronavirus at 43% for the majority of the population. However, one of the study's co-authors, Tom Britton of Stockholm University, believes that this model does not account for all sources of homogeneity.
“I believe that the difference will be larger, and the value of the required level of herd immunity will be less than 43%,” said Britton.
Another new studyuses a different approach to assess the difference in susceptibility to coronavirus, and further lowers the bar for herd immunity. The work has 10 authors, including Gomez and Langwig, and they estimate the threshold for herd immunity acquired naturally at 20%. If so, then in those parts of the world where the situation with the disease was the worst, they are already approaching this value.
“We conclude that the hardest hit regions like Madrid may already be close to herd immunity,” Gomez said. An early version of the work was published in May, and the authors are now working on an updated version, which is expected soon. It will show the herd immunity estimates for Spain, Portugal, Belgium and England.
That said, many experts consider these new studies - not all of which have yet been peer reviewed - as unreliable.
In a May Twitter thread, Dean emphasized that there is no certainty about many basic aspects of the disease - from different R 0 values in different conditions to the consequences of relaxing social distancing. Therefore, it makes no sense to trust the exact figures for the threshold value of herd immunity. This threshold can have one meaning when most people wear masks and avoid crowded places, and another, much higher when people are relaxing.
Other epidemiologists are also skeptical about low values. Jeffrey Shaman of Columbia University says the 20% herd immunity threshold “does not match respiratory viral infections. It doesn't fit the flu. So why should it be different for different respiratory viruses? I do not understand".
Miller adds: "I think the herd immunity threshold for naturally acquired immunity will be less than 60%, but I see no clear evidence that anywhere near this threshold."
In the end, the only way to truly get rid of the coronavirus pandemic is to achieve large herd immunity rates, everywhere, not just in the small number of places where the most people are infected. But this will most likely be possible only after the widespread distribution of the vaccine.
In the meantime, to prevent the spread of the virus and the maximum decrease in the value of R 0, you must observe social distancing, wear masks, get tested and track contacts everywhere, regardless of how you assess the herd immunity threshold.
“I don’t think I would have done anything differently if I knew that herd immunity value differs from the one I agree with, in the range of 40 to 60%,” Lipsic said.
The shaman also thinks that the uncertainty surrounding the herd immunity threshold, coupled with the consequences of misjudging it, leaves us with only one way out: to do everything possible to prevent new infections until we make a vaccine that allows us to safely reach herd immunity.
“The question is, will New York be able to withstand another outbreak? - he said. "I don't know, but let's not play with this fire."
See also: